Unraveling the Mystery of Confluent Hepatic Fibrosis: MRI Insights into Its Causes
2025-07-10
Author: Arjun
What is Confluent Hepatic Fibrosis?
Confluent hepatic fibrosis (CHF) is a benign condition marked by extensive scarring in the liver, potentially affecting one or multiple lobes and growing several centimeters thick. Despite its implications, the exact causes of CHF remain elusive, although it shares similarities with liver fibrosis.
Diverse Causes of Liver Fibrosis
Many factors contribute to liver fibrosis, including damage from viral hepatitis, schistosomiasis, tuberculosis, autoimmune hepatitis, and negative reactions to certain medications. Chronic liver damage, primarily from prolonged alcohol or drug abuse, stands out as the most prevalent culprit. Studies indicate that over 14% of patients with advanced cirrhosis develop CHF, predominantly linked to viral infections and chronic alcohol use.
The Role of MRI in Diagnosing CHF
Imaging techniques, especially MRI, are crucial for the non-invasive diagnosis of liver fibrosis. MRI is particularly beneficial for assessing CHF due to its detailed imaging and lack of harmful radiation. Magnetic resonance elastography is considered the most accurate method for detecting advanced liver fibrosis. However, CHF can sometimes mimic liver tumors, leading to possible misdiagnosis and unnecessary interventions.
Study Aim and Methodology
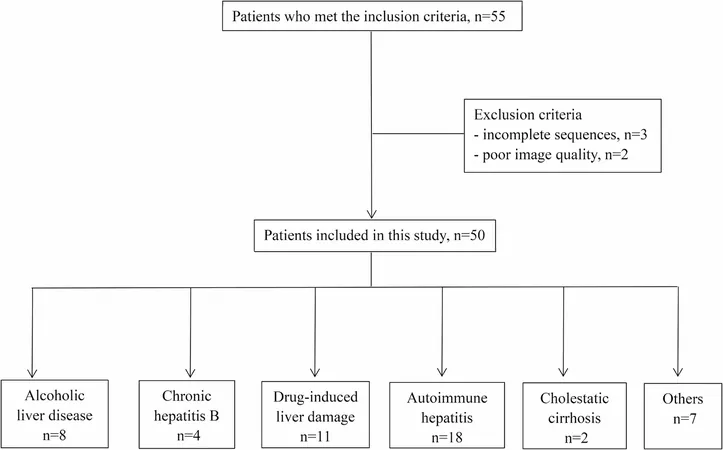
This study aimed to pinpoint key MRI features of CHF stemming from various causes to enhance clinical diagnosis. Researchers reviewed MRI data from patients diagnosed with CHF from January 2017 to July 2024, selecting individuals based on specific inclusion criteria to ensure accurate findings.
Profile of the Study Subjects
Fifty patients diagnosed with CHF were included, with detailed records of their sex, age, and liver disease history collected for analysis. Among the patients, there was a notable female majority, with various underlying causes identified, including autoimmune hepatitis and drug-induced liver injury.
Key MRI Findings
The MRI examinations revealed that 66% of CHF lesions exhibited a radial pattern around the liver's hilum, while the majority appeared patchy. Most lesions were hypointense on T1-weighted imaging but showed moderate hyperintensity on T2-weighted and diffusion-weighted imaging, supporting previous research.
Distinct Enhancement Patterns
In the late arterial phase of MRI, the lesions often showed mild to moderate enhancement, while most displayed heightened signals in the portal venous phase, particularly in alcoholic liver disease. These enhancement patterns provide essential insights for distinguishing CHF from other liver conditions.
Accompanying Findings and Implications
Many CHF lesions also coincided with liver cirrhosis and capsular retraction, factors that can complicate the diagnosis. Understanding these features can assist healthcare practitioners in differentiating CHF from malignancies like hepatocellular carcinoma, thus avoiding unnecessary biopsies.
Conclusions and Future Directions
This investigation sheds light on CHF's MRI characteristics across various etiologies, emphasizing the need for appropriate diagnostic protocols. Despite limitations inherent in the study's design, such as a small sample size, the findings pave the way for more comprehensive future research to further clarify the nuances of conclusive hepatic fibrosis and its management.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)