Unraveling the Dangers of Dengue: A Comprehensive Study of Pediatric and Adult Cases in Myanmar's 2022 Outbreak
2025-01-29
Author: Siti
Introduction
In recent years, dengue fever has emerged as a formidable public health threat globally, with a staggering 7.6 million cases reported to the World Health Organization (WHO) as of April 2024. Southeast Asia bears the brunt of this mosquito-borne viral disease, contributing approximately 70% of the total burden. Myanmar, a country in this region, experiences dengue epidemics every two to three years, with the most significant outbreak documented back in 1970. In 2015, the disease reached alarming proportions, affecting all seven states and regions nationwide, making the Yangon area, where Insein General Hospital (IGH) is located, a hotspot for dengue infections.
Understanding Dengue
Dengue is caused by four distinct viruses (DENV-1 to DENV-4), primarily spread by Aedes aegypti and Aedes albopictus mosquitoes. The symptoms can mimic other febrile illnesses, which often leads to misdiagnosis and delayed treatment, particularly when co-existing with diseases like COVID-19, Zika, or influenza. This makes it imperative to understand the clinical differences between dengue in children and adults, especially in a country like Myanmar, where various infections are prevalent during the rainy season.
The Study: Pediatric vs. Adult Dengue Cases at Insein General Hospital
Carried out during Myanmar’s 2022 dengue season (June to September), our research aimed to identify the clinical and virological differences between pediatric and adult dengue patients treated at IGH. The hospital serves as a treatment hub for multiple townships facing dengue outbreaks. With a significant patient base of 134 children (ages 1-12) and 87 adults (ages 13-54), the study focused on serotype identification, clinical severity, comorbid conditions, and the positivity rates of dengue infections.
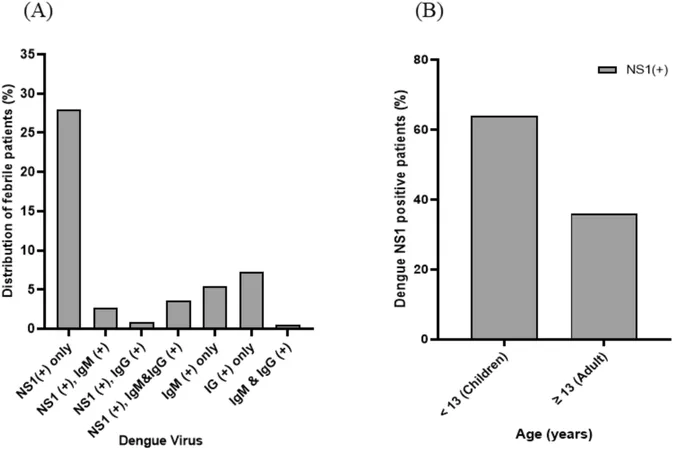
Key Findings: Current Dengue Landscape
From the 221 patients studied, 78 were found to be positive for dengue NS1 antigen (a marker indicating infection). Notably, DENV-1 emerged as the dominant serotype, accounting for nearly 68% of the cases, with a minor presence of DENV-2, DENV-3, and DENV-4. Both demographics exhibited similar positivity rates (37% in children, 32% in adults), underscoring an alarming trend: dengue, once considered primarily a children’s disease, now poses serious risks to adults too.
Symptomatology: Clinical Insights from the Field
The clinical manifestation of dengue varied between the two groups. In pediatric cases, the most frequent symptoms were high fever, vomiting, abdominal pain, and bleeding manifestations, with 12% experiencing dengue shock. Adults exhibited similar symptoms, but notably, muscle and joint pain was more prevalent among them. This may signal underlying health issues in adults—often with chronic conditions—with emphasized vigilance necessary to prevent misdiagnosis.
The Shadow of Comorbidities
Interestingly, the study found that dengue symptoms co-occurred with other diseases significantly more often in adults. This highlights the pressing need to diagnose and manage dengue comprehensively, especially when patients present with symptoms that could lead to a misdiagnosis.
The Road Ahead: Strategies for Managing Dengue in Myanmar
Given the cyclical nature of dengue outbreaks in Myanmar, the findings stress the importance of continuous monitoring of circulating serotypes. The predominance of DENV-1 and the occasional rise of DENV-2—known for its severe manifestations—should inform public health strategies. Furthermore, as adult dengue cases continue to rise, public health campaigns must shift to raise awareness among adults, reducing the stigma against visiting hospitals for mild symptoms. This study can serve as a blueprint for more extensive nationwide epidemiological research to adapt national guidelines effectively.
In summary, our research reveals that both pediatric and adult dengue cases share numerous clinical characteristics, yet coexisting conditions make adults particularly vulnerable. Health practitioners must remain vigilant for potential misdiagnoses during outbreaks—placing urgency on the examination and management of febrile patients, irrespective of their known medical histories. The time to act is now; strategies need to evolve to combat this increasingly pervasive threat!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)