Unmasking the Hidden Dangers: Hyperactive Delirium in Older Hospital Patients – A Major Threat!
2025-04-03
Author: Wei Ling
The Alarming Reality of Hyperactive Delirium in Older Patients
Recent research from Ramathibodi Hospital, Mahidol University sheds light on a troubling issue facing older medical inpatients: hyperactive delirium. With a staggering 48.3% of patients developing this condition during their hospital stay, the potential implications are alarming. Researchers sought to determine if hyperactive delirium significantly increases the risk of unexpected rehospitalization, ER visits, and mortality among older patients.
Study Overview and Findings
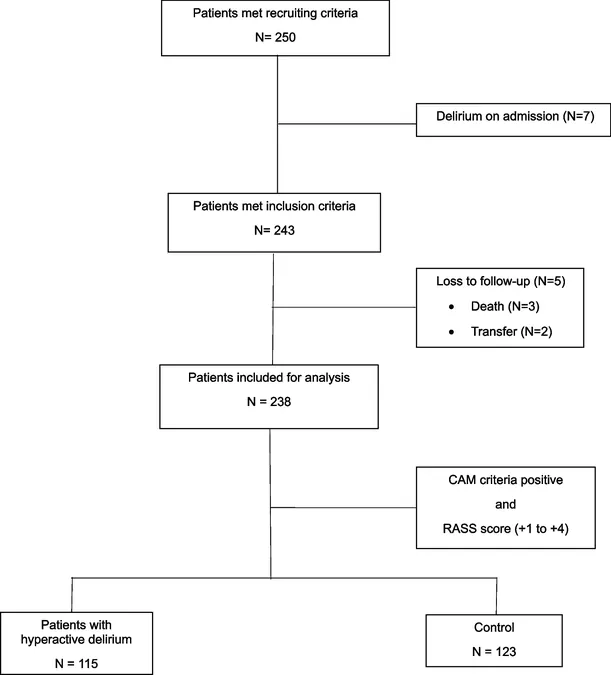
In a carefully designed prospective cohort study, 238 older patients (aged 60 and above) admitted to non-intensive care units from September 2022 to December 2023 were monitored for signs of hyperactive delirium—a condition characterized by heightened activity levels and confusion. Patients were evaluated upon their admission, with a sharp focus on their condition through daily assessments until discharge or death.
Key findings showed that those experiencing hyperactive delirium were more likely to be elderly, have lower educational levels, and exhibit frailty and cognitive impairments, significantly impacting their hospital stays and post-discharge outcomes. For instance, patients with hyperactive delirium faced an average length of stay of 7 days, compared to just 5 days for those without, highlighting the condition's serious impact on health care resources.
The Impact of Hyperactive Delirium
The consequences of hyperactive delirium can be severe. The study uncovered a stark contrast in mortality rates, with 12.2% of patients diagnosed with hyperactive delirium dying within 90 days of discharge, compared to only 1.6% in the control group. This drastic difference emphasizes the urgent need for healthcare providers to recognize and address this condition effectively.
Among the most concerning risk factors tied to hyperactive delirium were cognitive impairment (as indicated by a Montreal Cognitive Assessment score below 25), urinary incontinence, and frailty. Interestingly, conditions like congestive heart failure were also prominently associated with these patients, underlining how complex chronic diseases can interplay with delirium development.
A Call to Action: What Needs to Change?
The startling prevalence of hyperactive delirium compels a re-evaluation of treatment protocols for older patients in hospitals. This includes:
1. Better Screening Practices: Healthcare providers should routinely screen at-risk patients using validated tools like the CAM algorithm and the Richmond Agitation Sedation Scale to ensure early detection and intervention.
2. Medication Reviews: With polypharmacy identified as a significant factor in delirium risk, careful evaluation and necessary adjustments of medication protocols must be prioritized to minimize adverse drug effects.
3. Enhanced Staff Training: Training staff to recognize the signs of hyperactive delirium and understand its nuances is crucial for improving patient outcomes.
4. Long-term Follow-up Studies: More extensive research with longer follow-up periods is necessary to fully comprehend the long-term consequences of hyperactive delirium and improve preventive strategies.
As the healthcare community grapples with the implications of these findings, the spotlight remains on the significant dangers posed by hyperactive delirium in older hospital patients. Increased awareness and proactive measures can pave the way toward better health outcomes for this vulnerable population. By unmasking the hidden dangers of hyperactive delirium, we can seek to safeguard the health of our elderly patients, ensuring they receive the care they need during their most vulnerable moments.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)