Unlocking the Secrets of Neonatal Sepsis: The Power of Pentraxin-3 as a Diagnostic Tool
2025-03-24
Author: Nur
In a groundbreaking study that shines a light on neonatal health, researchers have delved into the diagnostic significance of Pentraxin-3 (PTX-3) alongside traditional infection markers such as C-reactive protein (CRP) and procalcitonin (PCT) in identifying neonatal sepsis. This research not only reveals compelling findings about the incidence of maternal premature rupture of membranes but also emphasizes the potential of PTX-3 as an early indicator of infection in newborns.
Key Findings: Maternal Premature Rupture of Membranes
The study revealed noteworthy statistics regarding maternal premature rupture of membranes (PROM). The sepsis group exhibited the highest PROM incidence at 22.86%, compared to 11.11% in the local infection group and just 2.63% in the non-infection cohort. These significant variances signal the vital role infections may play in the pathophysiology of PROM, suggesting that the presence of infection could compromise the integrity of membranes, leading to premature rupture and increasing the risk of poor neonatal outcomes.
Analyzing Infection Markers: WBC, PCT, CRP, and PTX-3
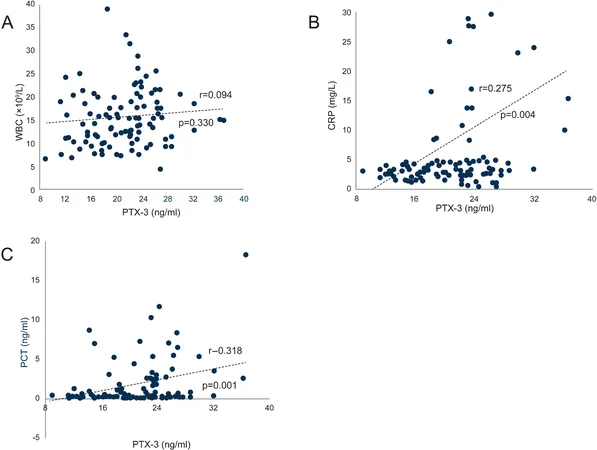
In comparing various biomarkers, the study found elevated white blood cell (WBC) counts in both the sepsis and local infection groups when set against the non-infection group. This confirms the expected heightened inflammatory response associated with infections. Among all the markers examined, PTX-3 emerged as a significant contributor, showing a strong correlation with CRP and PCT levels, demonstrating its potential as a reliable biomarker for neonatal infection.
Interestingly, while PTX-3 levels were significantly higher in the sepsis group, traditional metrics like WBC count did not correlate strongly with other inflammatory markers, suggesting that PTX-3 may provide a more nuanced picture of the inflammatory response in newborns.
The Diagnostic Revolution: The Impact of ROC Curve Analysis
ROC curve analysis underscored the diagnostic capabilities of PTX-3 when combined with other markers. The combination of PTX-3, CRP, PCT, and WBC demonstrated exceptional diagnostic performance for neonatal infections, boasting an impressive AUC (Area Under the Curve) of 0.954, indicating a sensitivity of 97.4% and a specificity of 83.1%. This is a significant leap in diagnostic accuracy, as early identification of neonatal sepsis is crucial for effective treatment.
Clinical Implications: Transforming Neonatal Care
The implications of these findings are profound. By identifying PTX-3 as a potential standalone marker for diagnosing neonatal infection, healthcare providers can pivot toward more effective diagnostic strategies. This could lead to faster diagnosis, timely interventions, and ultimately improved outcomes for vulnerable newborns.
Future Directions: Bridging Gaps and Expanding Research
Despite these encouraging results, the study acknowledges limitations, including a relatively small sample size of 109 neonates and the need for long-term follow-ups. Future research is essential to confirm PTX-3's diagnostic value across diverse neonatal populations and clinical settings. Furthermore, exploration of the biological mechanisms underlying PTX-3 responses, especially in context to factors like delivery mode and intrauterine distress, can provide deeper insights into its role in neonatal inflammation.
As we continue to unveil the mysteries behind neonatal infections, the integration of PTX-3 into clinical practice could mark a significant advancement in the early detection and management of neonatal sepsis, ultimately saving countless lives.
In summary, this study heralds a new era in neonatal diagnostics, reinforcing the critical need for further investigation into PTX-3 and its role in enhancing healthcare for our youngest patients.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)