Unlocking the Secrets of Metabolic Syndrome in Patients with MASLD: A Critical Study
2025-08-07
Author: Sarah
Exploring Metabolic Syndrome and MASLD: A Growing Concern
In an alarming trend, individuals with Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and type 2 diabetes mellitus (T2DM) are finding themselves at a higher risk for metabolic syndrome. A recent retrospective study, conducted at primary health care centers in the northern West Bank, scrutinized 240 diabetic patients diagnosed with MASLD to identify the predictive factors of metabolic syndrome.
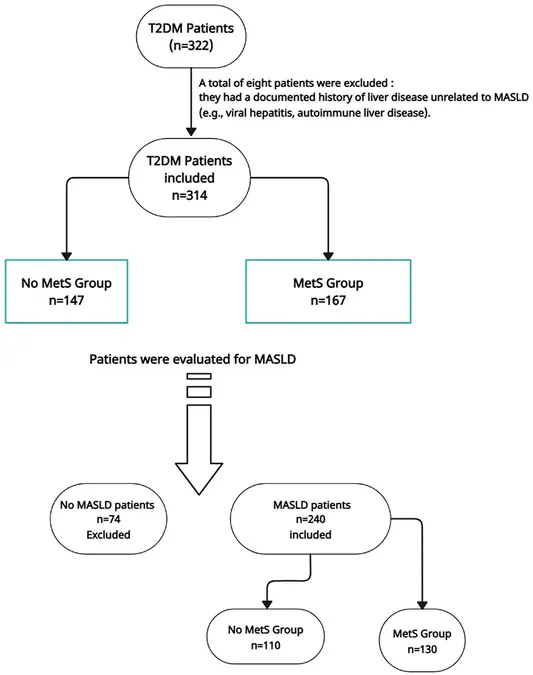
A Deep Dive into the Study Population
The study gathered data from a total of 314 patients, filtering out those without MASLD to focus solely on the most relevant cases. The resulting cohort underwent detailed assessments, including abdominal ultrasound examinations at various radiology centers. This meticulous approach ensured that only those with confirmed MASLD were evaluated, aiming for a representative sample of the affected population.
Understanding the Role of Diagnostic Tools and Definitions
MASLD was diagnosed through abdominal ultrasound and evaluated based on the Hepatic Steatosis Index (HSI), a non-invasive tool that relies on clinical markers like Body Mass Index (BMI) and liver enzyme levels. Metabolic syndrome was defined according to the reputable NCEP ATP III criteria, highlighting the interlinked criteria that classify patients into high-risk categories.
Unraveling Predictive Variables for Metabolic Syndrome
The study aimed to examine associations between a myriad of factors—sociodemographic data, clinical histories, metabolic profiles, and blood pressure readings—with the presence of metabolic syndrome. Results indicated that older age, greater waist circumference, dyslipidemia, and prolonged diabetes complications significantly predicted the likelihood of developing metabolic syndrome in MASLD patients.
Highlighting Key Findings: The Unmasking of Risk Factors
Key findings revealed that diabetic patients with metabolic syndrome exhibited significantly worse glycemic control, elevated blood pressures, and alarming lipid profiles. The study demonstrated that higher levels of systolic blood pressure and triglycerides correlated directly with increased odds of metabolic syndrome, whereas lower HDL cholesterol levels were linked to a higher risk.
The Impact of Diabetes Complications on Metabolic Health
Furthermore, the presence of diabetic complications—retinopathy, nephropathy, and neuropathy—were notably pronounced among those with metabolic syndrome. This affirms the notion that metabolic syndrome may exacerbate these conditions, creating a vicious cycle that demands immediate attention.
Recognizing Limitations and Future Directions
While the findings present critical insights, the study's cross-sectional nature limits causal assumptions. Future research is crucial to validate these results across diverse populations and to explore the intricate mechanisms through which these predictors operate. Such studies could enhance risk assessment tools and inform targeted interventions.
Concluding Insights: A Call to Action
As the number of MASLD and metabolic syndrome cases rises, understanding and identifying key risk factors becomes essential in creating effective screening and treatment protocols. This study not only confirms existing knowledge but also uncovers new correlates, urging both researchers and healthcare providers to prioritize this dual epidemic in clinical practice.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)