Unlocking the Secrets of Heparin: How Therapy Duration Affects Survival in Acute Pancreatitis!
2025-03-24
Author: Li
Introduction:
Acute pancreatitis is a life-threatening condition that often requires intensive care. One promising treatment option being explored is heparin therapy, known for its anticoagulant and anti-inflammatory properties. But the question remains—what is the ideal duration of heparin therapy to improve patient outcomes? A recent multi-center retrospective study has shed light on this critical issue, revealing shocking insights about how different durations of heparin therapy correlate with mortality in patients suffering from acute pancreatitis.
Objective:
The study aimed to determine the optimal duration of heparin therapy that minimizes mortality over 30 and 90 days in critically ill patients diagnosed with acute pancreatitis, a condition fraught with systemic complications.
Methodology:
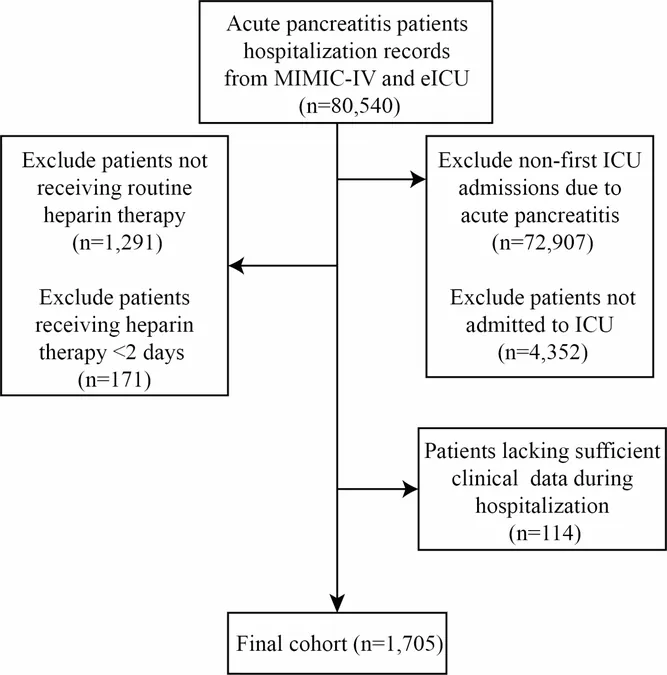
Utilizing data from prestigious databases—MIMIC-IV and eICU Collaborative Research Database—researchers analyzed records of 1,705 patients treated from 2008 to 2019. Four distinct groups were created based on the duration of heparin therapy: less than 4 days, 4 to 7 days, 8 to 14 days, and over 14 days. Advanced statistical methods, including restricted cubic splines (RCS) and Cox multivariate regression, allowed for a detailed comparison of mortality rates across these groups.
Results:
The findings unveiled a surprising J-shaped relationship between heparin therapy duration and mortality. Patients receiving heparin for around 7 days demonstrated the lowest rates of mortality—both at 30 days and 90 days. Strikingly, patients treated for fewer than 4 days exhibited a staggering 2.57 times higher risk of death within 30 days. Mortality rates stabilized beyond 7 days of therapy, underscoring the importance of adequate treatment duration.
Key Patient Characteristics:
The study also investigated various factors influencing patient outcomes, including age, sex, and common causes of acute pancreatitis such as gallstones and alcohol consumption. Those with heparin therapy lasting less than 4 days experienced significant complications across all demographic subgroups, highlighting a universal need for longer therapy durations.
Treatment Insights:
Among the patients analyzed, over 34% suffered from gallstone-induced acute pancreatitis. The study resonated with a growing body of evidence linking heparin to improved prognosis in critically ill patients. Observations suggested that heparin not only supports anticoagulation but also mitigates systemic inflammation, ultimately protecting pancreatic tissue from further injury.
What Do These Findings Mean?
This research emphasizes the critical importance of heparin therapy duration in managing acute pancreatitis. For patients in intensive care, a carefully monitored course of heparin lasting approximately 7 days could drastically improve survival chances. However, therapies shorter than this threshold increase the likelihood of mortality significantly.
Future Directions:
While the results are promising, they also prompt several questions for future research. Should there be new clinical guidelines specifically addressing personalized dosing strategies for different patient demographics? How can hospitals implement these findings effectively to enhance treatment protocols? Collaborative studies could further validate these results across broader and more diverse patient populations.
Conclusion:
The implications of this study are profound. Identifying optimal heparin therapy duration not only offers a beacon of hope for patients suffering from acute pancreatitis but also proposes a paradigm shift in our approach to treatment in critical care. As further research unfolds, it is vital to translate these findings into clinical practice, ensuring that medical professionals have the tools they need to save lives in the ICU.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)