Unlocking the Secrets of Early-Onset Alzheimer’s: Groundbreaking Genetic Predictive Model Revealed!
2025-05-05
Author: Sarah
Revolutionary Breakthrough in Alzheimer’s Prediction
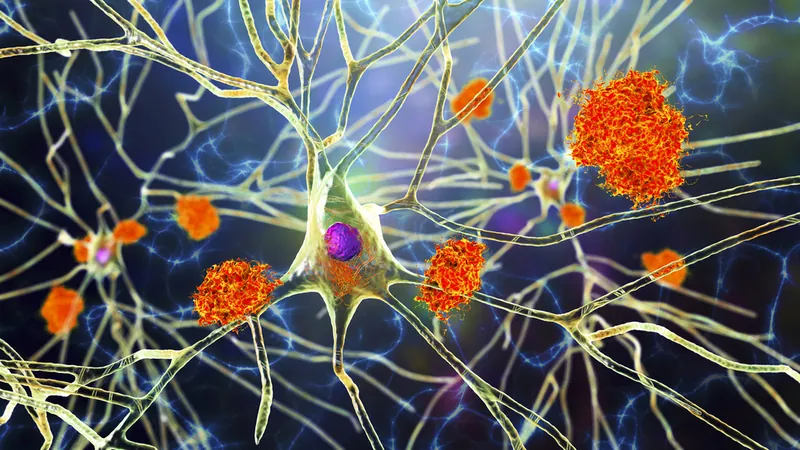
A team of brilliant researchers spearheaded by Lucía Chávez-Gutiérrez, PhD, at the VIB-KU Leuven Center for Brain & Disease Research has made a groundbreaking advancement in the fight against familial Alzheimer’s disease (AD). Their innovative method analyzes genetic mutations linked to amyloid-beta (Aβ) processing, offering a new way to predict the onset of this debilitating condition.
The Genetic Code: Understanding Disease Onset
Published in *Molecular Neurodegeneration*, this study uniquely connects biochemical changes in Aβ peptide profiles to specific genetic mutations within the PSEN1, PSEN2, and APP genes. This connection establishes a predictive model that could significantly enhance clinical diagnostics and shape future treatment strategies.
Chávez-Gutiérrez explains, “In cases of familial Alzheimer’s disease, patients often carry spontaneous genetic mutations, but until now, doctors were unable to offer precise information regarding these mutations. Our method provides a way to evaluate how likely a mutation is to trigger the disease and to forecast its onset.”
Diving Deep: Profiling Mutations and Their Impact
The research scrutinized 28 mutations in PSEN2 and 19 in APP, expanding upon previous findings that linked PSEN1 mutations to the early onset of symptoms. Familial Alzheimer’s disease is particularly aggressive, typically manifesting before age 65.
Past studies from Chávez-Gutiérrez’s lab revealed that PSEN1 mutations hinder γ-secretase enzyme activity, compromising its ability to convert Aβ peptides into less harmful forms. The current study delved into the PSEN2 and APP proteins, showing that similar dysfunctions in γ-secretase also correlate with earlier ages of onset.
The Research Unfolds: A Unified Model of Alzheimer’s Pathogenesis
Combining data from all three genes, the study discovered 'parallel but shifted lines,' revealing a common problem: γ-secretase dysfunction impacting disease timeline. This supports a cohesive model of Alzheimer’s pathogenesis, highlighting γ-secretase impairment and alterations in Aβ profiling as critical to disease onset.
The researchers quantified how different gene mutations influence the timing of symptom onset. Notably, mutations in PSEN2 delayed symptoms by an average of 27 years compared to PSEN1, while APP mutations postponed onset by eight years. According to Chávez-Gutiérrez, “A mere 12% adjustment in Aβ profile could potentially delay Alzheimer’s onset by up to five years.”
Personalized Medicine on the Horizon
This exciting new model not only provides estimations for age of onset but also helps identify mutation carriers whose clinical progression defies expectations, potentially shedding light on other genetic or environmental factors at play. “Our biochemical metrics offer crucial benchmarks to assess clinical age at onset (AAO) variability and the effectiveness of disease-modifying therapies,” the researchers highlighted.
Looking Ahead: New Therapeutic Strategies on the Horizon
While the research has made remarkable progress, the team noted limitations, particularly the less robust correlation for PSEN2 and APP mutations compared to PSEN1. This hints that additional factors, including transcript stability and environmental influences, could shape disease onset in certain individuals.
With these findings, the team envisions creating new therapeutic avenues for familial Alzheimer’s. Sara Gutiérrez Fernández, a doctoral researcher, remarked, “We have established a predictive model for age of onset that could lead to personalized strategies for managing familial Alzheimer’s. Future research will focus on developing therapies based on these predictions.”
The promise of personalized medicine shines brighter than ever in the fight against Alzheimer’s, and this groundbreaking research could be the key to unlocking new hopes for patients and their families.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)