Unlocking the Secrets of Ascites: Predicting Risks in Decompensated Cirrhosis Patients
2025-05-22
Author: Ming
Understanding Cirrhosis and Its Complications
Cirrhosis represents the final chapter of chronic liver disease, marked by severe liver damage. This condition progresses as dense fibrous tissue forms, altering liver functionality and leading to critical issues like increased portal vein pressure and symptoms of liver failure. One of the key indicators of deteriorating liver function is cirrhotic ascites—an accumulation of fluid in the abdomen that signals decompensation.
The Alarming Stats: How Common is Ascites?
Did you know? Approximately 58% of patients with initially compensated cirrhosis will develop ascites within just 10 years of their diagnosis. Once patients cross the threshold into hepatic ascites, the statistics reveal a staggering 15% mortality rate within the next year. Given that cirrhosis contributes to 2.4% of global deaths, the situation is dire, with around 10.6 million individuals worldwide suffering from this severe stage of the disease.
The Rising Economic Burden
In the U.S., patients suffering from cirrhosis and ascites face an average hospital stay of over five days, costing upwards of $42,000. The straining economic impact from this disease underscores the urgent need for effective management strategies.
Diagnosing and Treating Ascites: What's the Approach?
Ascites can be diagnosed through physical exams, imaging techniques, and fluid analysis. Treatment varies by severity, ranging from diuretics to more invasive measures like liver transplantation. Unfortunately, the prognosis often remains grim, which makes early prediction crucial for improving survival odds.
Investigating the Risk Factors
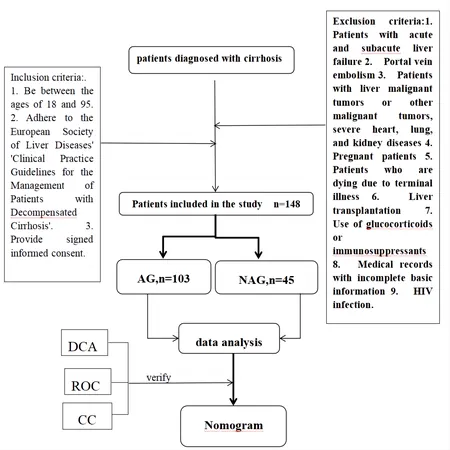
Recent research zeroes in on the risk factors contributing to ascites, with studies revealing complex interdependencies that impact findings. Through a comprehensive study conducted from July 2021 to November 2023, researchers at the Second Affiliated Hospital of Zhejiang University School of Medicine evaluated 148 patients, focusing on variables like age, gender, liver enzyme levels, and more.
Building a Better Predictive Model
The innovative aspect of this study is the creation of a predictive model utilizing a nomogram—an invaluable tool for clinicians. By analyzing clinical data, the researchers identified independent risk factors for ascites, revealing serum creatinine as a key predictor, while maintenance of albumin levels provided a protective effect.
Key Findings: What the Survey Revealed?
The findings are compelling. The patients with ascites displayed significantly lower albumin levels and increased serum creatinine levels. These results underscore the vital role of renal function and nutritional status in predicting ascites risk. Moreover, variations in Child-Pugh scores reflect the severity of liver dysfunction, correlating with increased likelihood of ascites.
A Call to Action
As we navigate the complexities of cirrhosis and its complications, this study emphasizes the urgent need for continuous research. With the integration of predictive analytics, healthcare professionals can identify high-risk patients earlier and implement timely interventions that could reshape the future of cirrhosis management.
Conclusion: The Path Forward
Ultimately, addressing the ascites challenge in decompensated cirrhosis not only improves patient care but also eases the economic burden on families and healthcare systems. By focusing on early detection and interventions, we can make significant strides against this formidable disease.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)