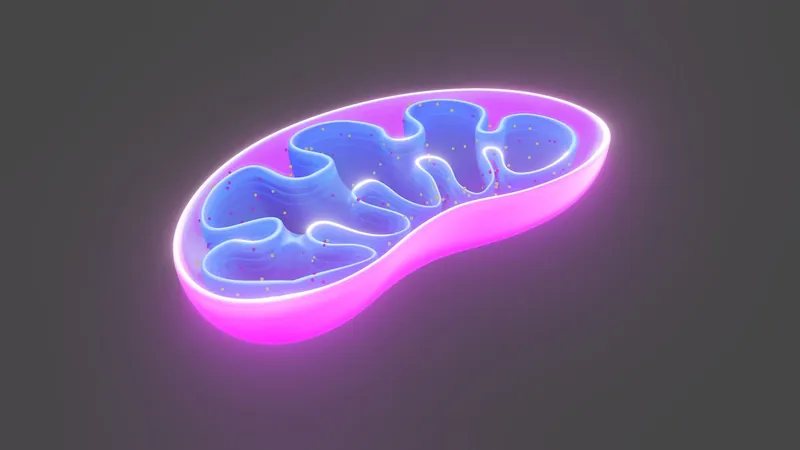
Unlocking the Secret: Mitochondria as Game-Changers in Treating Inflammatory Diseases!
2025-01-23
Author: John Tan
Groundbreaking Study on Mitochondria
In a groundbreaking study led by Dr. Navdeep Chandel and his research team, new insights into the role of mitochondria—often dubbed the cell's powerhouses—are emerging as potential allies in the fight against inflammatory diseases. Published in the distinguished journal Science Advances, this study sheds light on how mitochondria can significantly influence the body’s immune response by modulating critical cell signaling pathways.
Therapeutic Implications
Dr. Chandel, who is also a respected professor of Biochemistry and Molecular Genetics at Northwestern University, emphasizes the potential therapeutic implications of these findings. “Targeting mitochondrial function, especially within immune cells, could revolutionize treatments for a broad spectrum of inflammation-related conditions, including inflammatory bowel disease, sepsis, and chronic infections. Improving mitochondrial activity may enhance the immune system's capability to regulate inflammation effectively,” he stated.
Role of Mitochondria in Immune Response
Mitochondria play a vital role beyond merely producing energy in the form of ATP. They harbor the mitochondrial electron transport chain (ETC), a series of protein complexes essential for cellular energy metabolism. Notably, these protein complexes also regulate the function of macrophages, specialized immune cells crucial for combating infections and managing inflammation.
Significance of IL-10
These macrophages are responsible for releasing IL-10, an anti-inflammatory cytokine that not only curbs inflammation but also prevents harmful excess immune responses. However, prior to this study, the precise mechanisms by which the mitochondrial ETC influences macrophage responses remained elusive.
Research Findings
Using advanced bulk-RNA sequencing techniques to analyze mice with dysfunctional mitochondrial ETC complex III, researchers made a striking discovery: a specific type of reactive oxygen species (ROS) produced by this mitochondrial complex—known as superoxide—was essential for eliciting IL-10 production from macrophages. Fascinatingly, mice with impaired mitochondrial complexes showed difficulties in recovering from infections and inflammation due to inadequate IL-10 release. Fortunately, activating a certain ROS-dependent signaling pathway was found to restore IL-10 levels, showcasing the significant interplay between mitochondrial health and immune functionality.
Conclusion and Future Directions
This research reveals a previously uncharted relationship between mitochondrial operations, inflammation management, and the signaling pathways that govern these processes,” remarked Dr. Chandel. The implications of these findings are vast. By illuminating the pivotal role of mitochondria in inflammation-related pathways, this research points to mitochondria as a highly promising therapeutic target. Enhancing mitochondrial performance could transform therapeutic strategies for various inflammatory disorders, potentially leading to better outcomes for patients battling these perplexing diseases.
As research continues in this exciting field, the medical community stands on the brink of potentially rewriting the rulebook on how inflammatory conditions are managed, igniting hope for many who suffer from chronic inflammatory diseases. Stay tuned for more updates on this revolutionary approach that could change lives!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)