Unlocking the Mystery of Liver Fibrosis: PDGFRβ as a Game-Changing Non-Invasive Biomarker for Diabetic Patients
2025-07-17
Author: Yu
A Global Health Crisis: The Rise of Metabolic-Associated Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD), now more accurately termed metabolic-associated fatty liver disease (MAFLD), is sweeping across the globe, affecting 25-30% of the population. This alarming trend correlates with the worldwide epidemic of obesity and type 2 diabetes mellitus (T2DM). MAFLD is characterized by excessive fat in the liver without significant alcohol consumption, and its impacts extend beyond mere liver health, leading to severe outcomes like cirrhosis and cancer.
The Challenges of Diagnosing MAFLD
Despite being critical, diagnosing MAFLD often relies on liver biopsies, the gold standard for assessing fibrosis. Yet, these procedures are invasive and carry risks, making them unsuitable for widespread use. This highlights an urgent need for reliable non-invasive biomarkers to accurately monitor liver health.
Why Diabetics are at Greater Risk
Patients with T2DM face a heightened risk of MAFLD and its more pernicious form, metabolic-associated steatohepatitis (MASH). Current clinical guidelines recommend regular screening using less invasive methods, yet results remain inconsistent, particularly for diabetic patients. Many tests have shown poor performance when applied to this specific group.
The Promise of PDGFRβ as a Biomarker
Recent research has put a spotlight on platelet-derived growth factor receptor-beta (PDGFRβ) as a potential non-invasive biomarker. In healthy livers, PDGFRβ levels are low, but they spike dramatically during liver injury, signaling fibrogenesis. Studies indicate that PDGFRβ could revolutionize how we assess liver fibrosis in diabetic patients grappling with MAFLD.
What the Numbers Say: Key Findings on PDGFRβ
In a comprehensive study involving 90 MAFLD patients—50 diabetic and 40 non-diabetic—significantly elevated PDGFRβ levels were observed. Diabetic patients faced a higher degree of liver steatosis and fibrosis compared to their non-diabetic counterparts. Notably, PDGFRβ showed impressive diagnostic accuracy for significant liver fibrosis (≥ F2) with a staggering specificity and sensitivity.
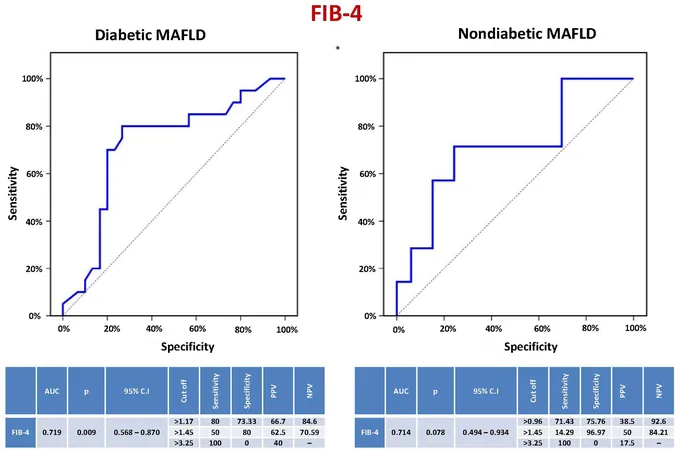
Combining Forces: PDGFRβ and FIB-4 for Enhanced Diagnostics
When combined with the FIB-4 score, PDGFRβ demonstrated even greater predictive power, achieving 100% sensitivity in identifying significant fibrosis among diabetic patients. This dual approach could significantly reduce the need for invasiveness while enhancing diagnostic accuracy.
Moving Forward: Implications for Patient Care
In Egypt, where MAFLD prevalence reaches about 47.5%, reliable biomarkers like PDGFRβ could be instrumental in guiding treatment decisions. By accurately identifying patients at risk for significant fibrosis, healthcare providers can tailor monitoring and treatment strategies, ultimately improving patient outcomes.
Conclusion: A Potential Breakthrough in Liver Care
This study underscores the importance of innovative diagnostic approaches in managing MAFLD, particularly among diabetic patients. By leveraging PDGFRβ, we could take a step closer to non-invasive fibrosis assessments, paving the way for better healthcare solutions and outcomes in the fight against liver disease.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)