Unlocking the Mystery of Antibiotics: How They Work and the Rise of Resistance
2024-12-23
Author: Rajesh
The Mechanisms of Antibiotics
Antibiotics are classified into various types, each designed to target specific bacterial functions or structures. For example:
- **Beta-lactam antibiotics** (like penicillin) focus on disrupting the production of the peptidoglycan layer, essential for bacterial cell walls. This results in weakened walls, ultimately leading to the bacterium’s demise.
- **Tetracyclines**, on the other hand, inhibit bacterial growth by binding to ribosomes, the cellular machinery responsible for protein synthesis. This makes these antibiotics effective against both Gram-positive and Gram-negative bacteria.
Interestingly, many of our current antibiotics are derived from natural sources. Certain bacteria produce these compounds to outcompete neighboring bacteria in their environment, creating an evolutionary arms race where resistance is a critical survival skill.
The Evolution of Resistance
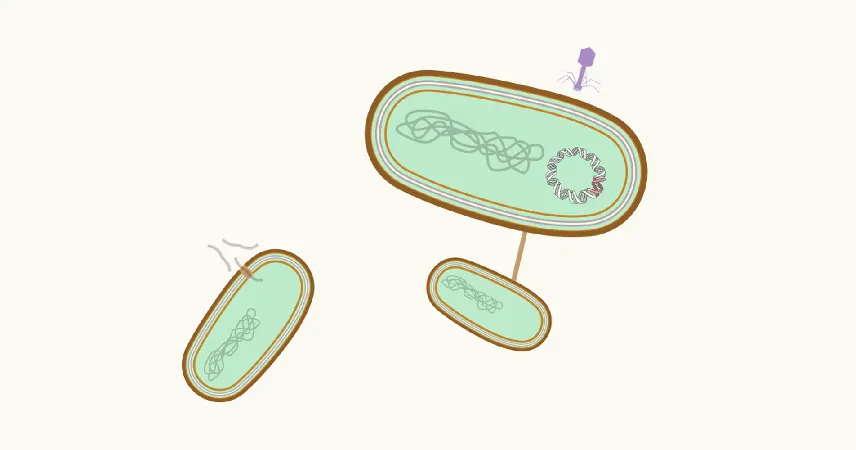
Bacteria are notorious for their adaptability. They can quickly develop and share resistance mechanisms through several processes:
1. **De Novo Innovations:** Random mutations in DNA can lead to new traits, including antibiotic resistance.
2. **Horizontal Gene Transfer:** Bacteria can acquire resistant genes from one another through methods such as conjugation (direct transfer), transduction (involving viruses), or transformation (absorbing DNA from their surroundings).
Moreover, some bacteria can forge beneficial relationships with others, gaining survival advantages from their interactions. They can also spread through populations and environments, making containment a challenge.
Despite these resistant strains being remarkably resilient, they often face trade-offs. Developing mechanisms like beta-lactamases to counteract antibiotics requires energy—sometimes hampering their growth. This means that some bacterial species, like those causing syphilis, may still remain susceptible to certain antibiotics like penicillin, due to a lack of viable resistance strategies.
Understanding the Pace of Resistance Development
The rate at which resistance develops varies. Laboratory settings can observe resistance emerging within days, but in the real world, the process is slower—taking weeks to months in individual patients and even longer across populations.
Antibiotic use exerts consistent selection pressure, leading to the emergence of resistant strains. It's essential, therefore, to use these medications judiciously to maintain their effectiveness and delay the emergence of resistance.
Hope for the Future: New Strategies Ahead
To tackle antibiotic resistance, researchers are exploring innovative strategies and technologies designed to make it more difficult for bacteria to develop resistance mechanisms. Some approaches include:
- **Combination Therapies:** Using two or more antibiotics can sometimes prevent the development of resistance, as bacteria would need to overcome multiple mechanisms simultaneously.
- **New Antibiotic Classes:** Developing new classes of antibiotics that bacteria have yet to encounter could provide a significant advantage.
The ongoing arms race between antibiotics and bacteria requires vigilance and adaptability from the medical community. By understanding these dynamics, we can make strides in preserving the effectiveness of antibiotics and ensure they continue to save lives.
In conclusion, while the threat of antibiotic resistance is real and growing, understanding the mechanisms of antibiotics and resistance can empower us to develop more effective treatments and strategies for managing bacterial infections. With collective effort and research, we can hope to spark a new renaissance in antibiotic development and usage.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)