Unlocking Diabetes: How Your Body Clock Affects Metabolic Health
2025-04-17
Author: Wei Ling
Recent groundbreaking research from Northwestern Medicine highlights a striking connection between circadian rhythm disruptions and metabolic diseases like diabetes. This compelling study was featured in the prestigious Proceedings of the National Academy of Sciences.
Dr. Clara Peek, a lead author and an expert in Biochemistry and Molecular Genetics, warns that environmental disruptions—such as shift work, jet lag, or lack of sleep—can disturb our internal body clocks. By disrupting these biological rhythms and combining them with poor dietary choices, we may increase our risk for developing glucose intolerance and eventually, diabetes.
The Science Behind Your Body’s Clock
Our body's circadian clock, governed by proteins known as transcription factors, plays a vital role in syncing physical and behavioral changes to our 24-hour day. While past research has linked circadian disruptions to metabolic conditions, the specific role of muscle tissue's internal clock has remained largely unexplored.
In an innovative study, Peek's team investigated how these circadian rhythms affect muscle metabolism—specifically how muscles convert glucose into energy. The research focused on mice bred without the BMAL1 gene, a key regulator of both circadian rhythms and muscle function.
Staggering Findings Revealed in Mice Experiments
The results were astonishing. Mice on a high-fat, high-carb diet displayed severe glucose intolerance even without significant weight gain, highlighting that the absence of the BMAL1 gene exacerbated diabetic symptoms.
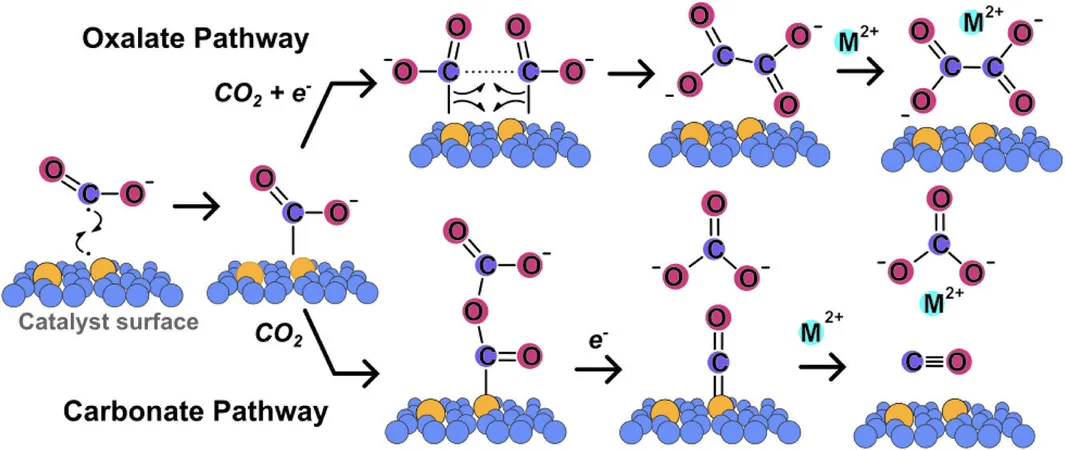
Further analysis revealed that the muscles of these genetically altered mice had serious disruptions in glucose utilization during early glycolysis, the process that converts glucose into cellular energy. This demonstrates that the internal clock within our muscle tissue plays a crucial role in metabolic health.
A Ray of Hope: Reversing Glucose Intolerance
Intriguingly, the researchers found that during instances of diet-induced obesity, BMAL1 collaborated with the hypoxia-inducible factor (HIF) pathway to adapt muscle metabolism to nutrient stress. By restoring HIF activity in muscles lacking BMAL1, researchers successfully reversed glucose intolerance—offering a potential avenue for future therapies.
Dr. Peek emphasized the significance of these findings, stating, "Disrupting the muscle clock loses its connection with HIF, leading to impaired glucose metabolism. Understanding this connection could be a game-changer in diabetes management."
What’s Next? The Path Forward
As the team gears up for further exploration, they aim to determine if circadian rhythms are disrupted in animal models of diet-induced obesity. They are particularly interested in how these disruptions impact glucose intolerance and insulin resistance, ultimately contributing to our understanding of diabetes.
In a world where lifestyle factors heavily influence health, this research sheds light on the importance of maintaining a balanced body clock for metabolic well-being. The implications could be vast—for both personal health and large-scale public health policies.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)