
Unlocking Access: How School-Based Health Centers Could Revolutionize Children's Vaccination Rates
2025-04-17
Author: Daniel
In a shocking revelation, vaccination rates for children have plummeted below critical levels in over 8,000 schools across the United States, and it’s not just due to vaccine hesitancy. A health policy expert from Texas A&M University, Dr. Simon Haeder, sheds light on the alarming factors contributing to this decline.
“The outbreaks of measles and other preventable diseases we're witnessing today are a direct result of these lowered vaccination rates,” warns Haeder. The real issue, he says, often lies in the significant lack of access to healthcare, particularly impacting racial and ethnic minorities, low-income families, and those living in rural areas.
A stark national study from 2022 highlighted this issue: Hispanic and Black children were reported to have markedly lower rates of preventive care visits compared to their non-Hispanic white counterparts, revealing a troubling gap influenced by socioeconomic status.
In a groundbreaking study, Dr. Haeder investigated public sentiment towards school-based health centers—an established option that caters to over 6.3 million K-12 students across the country. Published in *World Medical & Health Policy*, this assessment is a first of its kind.
These centers not only provide vaccinations but also offer a broad spectrum of health services, including care from advanced practice nurses, physicians, mental health specialists, and even vision and dental care. They're a powerful tool in increasing vaccination rates, yet public perception and hesitancy surrounding vaccinations have remained largely unexplored until now.
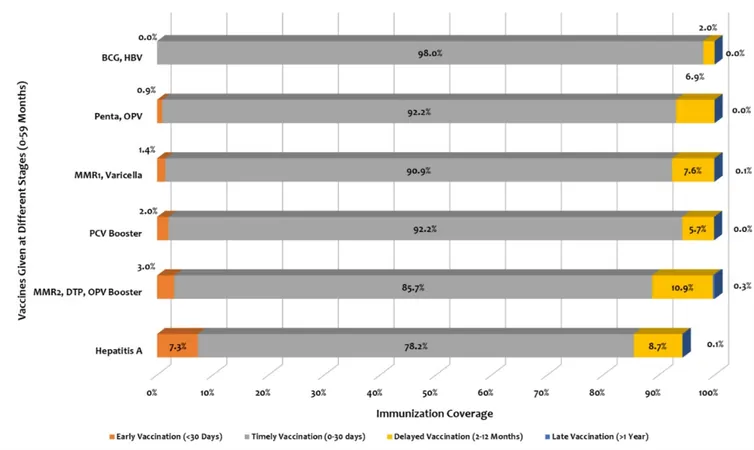
Dr. Haeder surveyed a nationally representative sample of 4,196 individuals, querying their opinions on seven vaccines commonly available through school-based health centers: DTaP, polio, chickenpox, MMR, hepatitis, HPV, and COVID-19. Respondents discussed their political views, trust in school leadership, and general attitudes towards vaccinations.
The findings revealed substantial public support for these vaccination services, with approval ratings ranging from 73.6% for COVID-19 to a striking 84.2% for MMR. This is particularly noteworthy in a time of widespread disagreement on health issues across the nation.
Key factors influencing this support included political ideology, trust in school principals, and prevalent measures of vaccination hesitancy—illustrating that such hesitancy significantly affects public perceptions of immunization.
Haeder emphasizes the need for further research on decision-making related to the vaccination services offered in school-based health centers, which could greatly inform future health policy developments.
As we face an ongoing battle against preventable diseases, the expansion and support of school-based health centers may prove vital in ensuring our children receive the vaccinations they need to stay safe and healthy.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)