Unleashing the Power of Adoptive Cell Therapy Against Malignant Melanoma: A Hopeful Frontier in Cancer Treatment
2025-01-22
Author: Wei
Melanoma: An Evolving Challenge
Melanoma, particularly cutaneous melanoma, stands as one of the most aggressive and lethal forms of skin cancer. The grim statistics reveal that this type of melanoma constituted about 1.6% of all cancers and was responsible for over 60,000 deaths globally in 2018 alone. Alarmingly, while many other cancers are witnessing a decline or plateau in incidences, melanoma rates have been persistently on the rise. Early detection is crucial, and skin biopsy remains the gold standard for diagnosis, supplemented by innovative molecular and imaging techniques. However, around 3% of melanoma cases are classified as melanoma of unknown primary (MUP) – a puzzling form of the disease that poses unique diagnostic challenges.
Recent advances in cancer therapy have pivoted towards checkpoint inhibitor immunotherapy, utilizing agents like anti-PD1 (nivolumab, pembrolizumab) and anti-CTLA4 (ipilimumab) antibodies, which have shown promise in treating advanced melanoma. Nevertheless, many patients develop resistance over time, emphasizing the urgent need for more effective treatments. Enter the world of microRNAs (miRNA) – small molecules that are emerging as potential allies in making melanoma cells more susceptible to existing immune checkpoint therapies.
However, the conventional treatments face significant limitations due to immune suppression in the tumor microenvironment (TME). Key players like M2 macrophages, regulatory T cells (Tregs), and myeloid-derived suppressor cells (MDSCs) play destructive roles by altering immune responses that can thwart treatment efforts. Soluble factors, such as interleukin-10 and TGF-β, further complicate the immune landscape, contributing to poor treatment outcomes and high recurrence rates.
Adoptive Cell Therapy: A Beacon of Hope
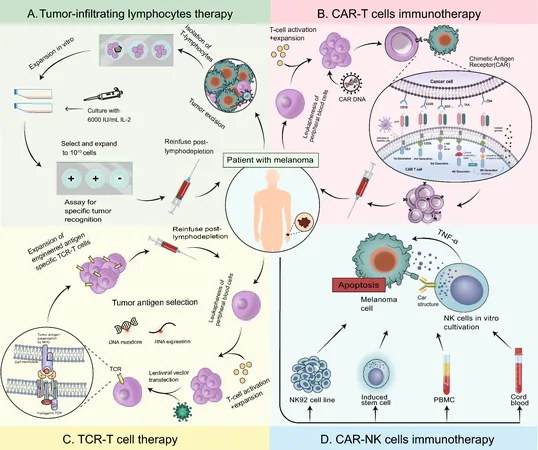
Adoptive Cell Therapy (ACT) has emerged as a revolutionary approach in the fight against melanoma. This therapy involves the extraction of a patient’s immune cells, particularly T cells, augmenting their tumor-fighting capabilities through modification and expansion before reintroducing them into the patient. By directly addressing issues associated with immune suppression, ACT holds promise for both hematologic malignancies and solid tumors like melanoma.
Among the most prominent ACT strategies is Tumor-Infiltrating Lymphocyte (TIL) therapy. This involves isolating immune cells that have naturally infiltrated tumors and expanding them in culture before re-infusion. TILs are particularly effective due to their specificity to tumor antigens. However, the manufacturing and expansion of these cells pose significant challenges, leading to innovative solutions like magnetic affinity targeting of infiltrating cells (MATIC) technology, which streamlines the sorting process.
Clinical trials have demonstrated remarkable success. For instance, one study reported a 56% objective response rate for TIL therapy, reinforcing its potential as a viable treatment option for patients with advanced melanoma. The FDA has recognized the efficacy of TIL-based therapies by granting fast-track designations, paving the way for promising new treatments to reach patients sooner.
In parallel, researchers are exploring the potential of Chimeric Antigen Receptor T-cell (CAR-T) therapy for melanoma. By genetically engineering T cells to express a receptor that targets specific melanoma antigens, CAR-T therapy aims to activate a potent anti-tumor response, unbound by human leukocyte antigen (HLA) restrictions. While clinical trials specifically focused on melanoma are still sparse, initial studies showcase the dream of utilizing CAR-T cells against this formidable cancer.
Furthermore, the innovative T-cell receptor (TCR) therapy method offers hope by genetically engineering T cells to specifically identify and attack melanoma cells, even those traditionally difficult to target through other methods. Initial investigations have yielded encouraging results, but challenges such as off-target toxicity and potential neurotoxic effects remain pressing issues that researchers are keen to address.
The future of CAR-NK therapy, utilizing natural killer cells engineered with CARs, also looms brightly on the horizon. These cells may offer an off-the-shelf treatment option free from the complications seen with T cells. Despite a current lack of extensive clinical trials specifically addressing its efficacy in melanoma, the promising results in other solid tumors may pave the way for its introduction in melanoma treatment protocols.
Conclusion: A Future Filled with Promise
As scientists unveil new therapeutic strategies, including the likes of ACT in various forms, melanoma treatment stands at a hopeful juncture. With ongoing research focusing on minimizing limitations like treatment resistance and exploring innovative engineering methods, the landscape of melanoma therapy is evolving rapidly. The goal is not only to enhance survival rates but also to ultimately transform malignant melanoma from a dreaded diagnosis into a more manageable condition—fully reclaiming lives that cancer has sought to take away. Stay tuned, as the battle against melanoma may witness groundbreaking victories in the years to come!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)