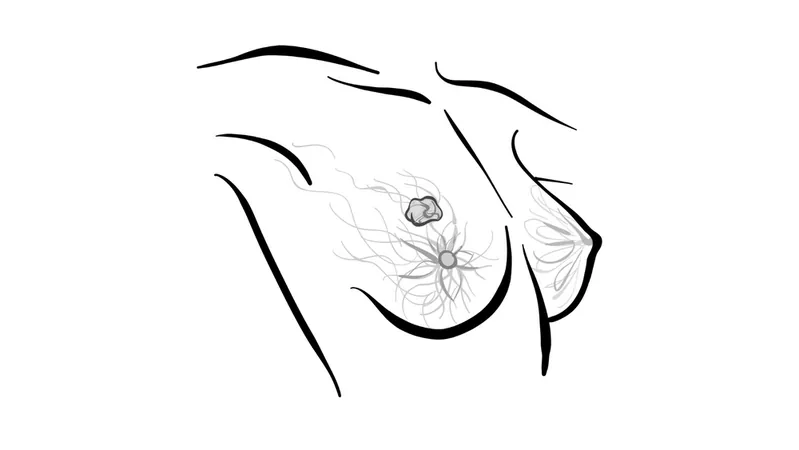
Understanding the Impact of TROP2 and HER2 Status on Sacituzumab Treatment in Hormone-Receptor Positive Metastatic Breast Cancer
2024-09-26
In the realm of metastatic breast cancer (mBC), defining endocrine resistance is crucial for determining treatment pathways. Dr. Wei shares insights on assessing endocrine resistance, delineating between primary and secondary resistance. Primary resistance occurs in patients relapsing within the first year of adjuvant endocrine therapy, while secondary resistance is noted if relapse happens after the first two years or within a year post-therapy. This distinction is vital for tailoring appropriate treatment plans.
For patients grappling with hormone receptor-positive, HER2-negative metastatic disease, treatment options include trastuzumab deruxtecan (T-DXd) and sacituzumab govitecan (Trodelvy). Guidelines from the National Comprehensive Cancer Network (NCCN) stipulate that sacituzumab should be considered after patients have undergone at least two systemic therapies, which may include specific chemotherapies. The FDA, however, emphasizes prior chemotherapy in the metastatic setting as a stricter criterion for sacituzumab use.
The phase 3 TROPiCS-02 trial is shedding light on the effectiveness of sacituzumab in patients with advanced ER+ breast cancer. Enrolling over 500 participants, the trial required previous treatment with at least one line of endocrine therapy, a taxane, and a CDK4/6 inhibitor. Results revealed a median progression-free survival (PFS) of 5.5 months for sacituzumab compared to 4.0 months for the treatment of physician's choice (TPC). Additionally, median overall survival (OS) figures are striking, with sacituzumab achieving 14.4 months compared to 11.2 months for TPC.
An intriguing aspect of these findings is the role of TROP2 expression levels. The exploratory analysis from the ASCENT trial suggests that higher TROP2 expression correlates with improved overall response rates (ORR) and longer PFS. Patients with high TROP2 levels exhibited response rates as high as 44%, compared to only 1% in the lowest category. Meanwhile, HER2 status also plays a notable role in treatment outcomes. In HER2-low settings, sacituzumab achieved a median PFS of 5.8 months versus 4.2 months for TPC, further emphasizing the importance of this biomarker.
Additionally, researchers are probing the implications of sequential treatment with sacituzumab and T-DXd. Data suggest that regardless of the order in which these antibody-drug conjugates are administered, the second ADC tends to yield shorter PFS. Consequently, this raises vital questions regarding treatment sequencing in advanced breast cancer regimens, especially as more ADCs like datopotamab deruxtecan are introduced.
However, the safety profile of sacituzumab cannot be overlooked. While it improves OS, a significant percentage of patients experienced grade 3 or higher adverse events (74% with sacituzumab versus 60% with TPC), with neutropenia and diarrhea being the most commonly reported side effects.
In conclusion, as therapeutic strategies evolve for hormone receptor-positive metastatic breast cancer, understanding the interplay of TROP2 and HER2 status with treatments like sacituzumab is essential for optimizing patient outcomes. With ongoing research shedding light on these critical factors, there is potential for enhancing treatment personalization and improving survival rates for this challenging patient population.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)