Uncovering the U-Shaped Link Between Stress Hyperglycemia Ratio and Mortality in NAFLD Patients
2025-07-01
Author: Ming
A Deep Dive into NAFLD and the Significance of the Stress Hyperglycemia Ratio (SHR)
Recent research has exposed an intriguing U-shaped relationship between the Stress Hyperglycemia Ratio (SHR) and mortality rates in patients with Non-Alcoholic Fatty Liver Disease (NAFLD). This ground-breaking study utilized data from the National Health and Nutrition Examination Survey (NHANES), shedding light on how hyperglycemia, both acute and chronic, affects longevity in NAFLD patients.
Understanding the NHANES Study and its Findings
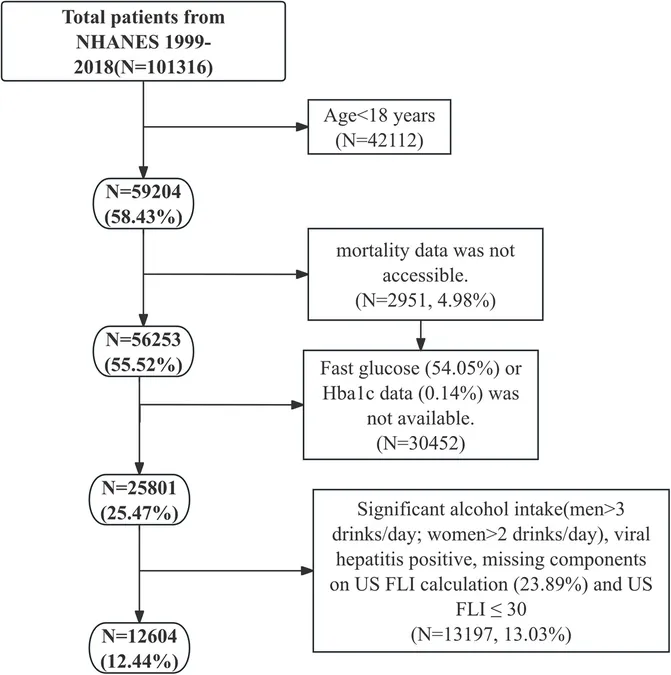
The NHANES dataset, which captures a representative sample of the U.S. population, served as the foundation for this analysis. Researchers sifted through data collected between 1999 and 2018, ultimately narrowing their focus to 12,604 eligible participants diagnosed with NAFLD using a non-invasive scoring system known as the United States Fatty Liver Index (US FLI). This method circumvents the challenges posed by traditional biopsy, which can be both invasive and expensive.
Decoding NAFLD and Its Diagnostic Challenges
With NAFLD affecting millions, diagnosing it accurately is critical yet complex. The US FLI score, developed from a combination of easily measurable clinical variables—like waist circumference and liver enzyme levels—was employed to estimate the presence of hepatic steatosis, a hallmark of NAFLD.
The Mystery of Stress Hyperglycemia Ratio (SHR)
SHR is calculated with a formula comparing fasting blood glucose levels to hemoglobin A1c (HbA1c) values. By stratifying patients into four SHR quartiles, the study aimed to explore how fluctuations in blood sugar impact mortality risk.
Mortality Rates and the U-Shaped Association
Astoundingly, results revealed a U-shaped correlation between SHR and all-cause mortality rates. Patients in the middle quartile had the lowest mortality risk, while both low and high SHR levels were linked to increased mortality. This relationship became particularly pronounced among middle-aged and older adults, prompting researchers to suggest that optimal SHR levels may mitigate risks associated with NAFLD.
Significance of Results Across Different Age Groups
Age-stratified analysis highlighted that individuals aged 40-59 and 60-85 exhibited significant mortality risks associated with extreme SHR levels. Inflection points were identified at SHR values of 0.89 for middle-aged groups and 0.94 for older adults, marking optimal thresholds for minimizing risk.
Implications for Clinical Practice and Future Research
These findings underscore the importance of tailored interventions aimed at maintaining SHR within optimal ranges to enhance patient health outcomes. The study advocates for dynamic glycemic management strategies while calling for further research to corroborate these results across diverse populations and settings.
Conclusion: A Game Changer in NAFLD Management?
As we unravel the complexities of NAFLD, the U-shaped association between SHR and mortality introduces captivating questions about glycemic management. Enhancing our understanding of this relationship could revolutionize treatment strategies for millions suffering from NAFLD, emphasizing the crucial role of maintaining balanced blood sugar levels in promoting longevity and health.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)