Uncovering the Truth: How Weight Loss Can Transform the Lives of Women with Polycystic Ovary Syndrome!
2024-11-04
Author: Wei
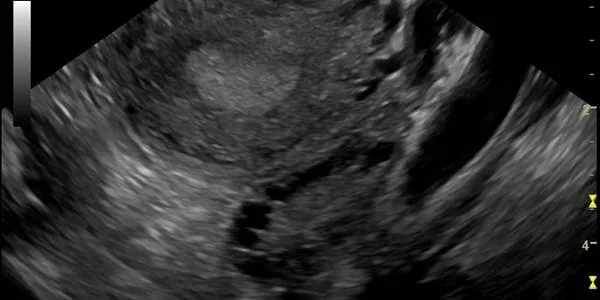
In a groundbreaking systematic review and meta-analysis, researchers have unveiled that weight loss interventions can significantly enhance metabolic and reproductive outcomes for women battling Polycystic Ovary Syndrome (PCOS). With more than half of the women suffering from PCOS being overweight or obese, the implications of this study are vital for the estimated 5 to 10 percent of women affected by this hormonal disorder, which can cause a myriad of health issues ranging from infertility to metabolic syndrome.
The study showed that those who engaged in targeted weight loss programs experienced a remarkable decrease in insulin resistance and free androgen index (FAI), alongside a substantial increase in the frequency of menstruation. Specifically, participants lost an average of nearly 4 kilograms, reducing fasting insulin levels significantly, although fasting glucose levels remained unaffected.
What Does This Mean for Women?
Clinical guidelines currently recommend weight loss as a primary intervention for women with PCOS. However, mere advice is often ineffective as many women struggle to implement consistent lifestyle changes. This study pushes for more structured weight loss programs—ranging from dietary adjustments and physical activity to pharmacotherapy and even bariatric surgery—as essential remedies to combat the symptoms of PCOS.
The findings suggested that these interventions can lead to a decrease in key hormonal markers: - A drop in insulin resistance mobility was noted, with a mean difference of -0.45 in the primary outcomes. - FAI levels decreased by approximately 2.03 points. - Menstruation frequency among participants on weight loss interventions increased, averaging an additional 2.64 cycles per year.
Despite these promising results, the study did indicate that adverse effects related to gastrointestinal issues occurred more frequently among those on weight loss interventions. Therefore, while the results are compelling, potential risks should not be overlooked.
Limitations and Future Directions
The study’s generalizability is tempered by its use of various interventions and some high-risk biases within the trials examined, pointing to a need for more uniform research methods in future studies. Nonetheless, this significant research underscores the need for integrated weight management approaches tailored for women with PCOS to improve not only physical but also emotional well-being.
For women navigating the challenges of PCOS, these findings are an encouraging sign that with the right support and interventions, significant improvements can be achieved in their health trajectories.
Could the key to unlocking a healthier, reproductive future lie in weight management? Women with PCOS may want to explore these interventions to regain control over their bodies and lives! For more detailed insights, stay tuned as we continue to follow the latest research in health and women's issues.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)