Uncovering the Hidden Risks: Predictors of Self-Reported Hypertension Among Women of Reproductive Age in North Dakota
2025-01-03
Author: Li
Introduction
Hypertension is often dubbed the "silent killer," especially among women of reproductive age (18-44 years). Identifying the risk factors leading to high blood pressure in this demographic is crucial for shaping effective health initiatives aimed at reducing hypertension-related complications. A recent study aimed to uncover predictors of self-reported hypertension among women in North Dakota, revealing startling insights.
Methodology
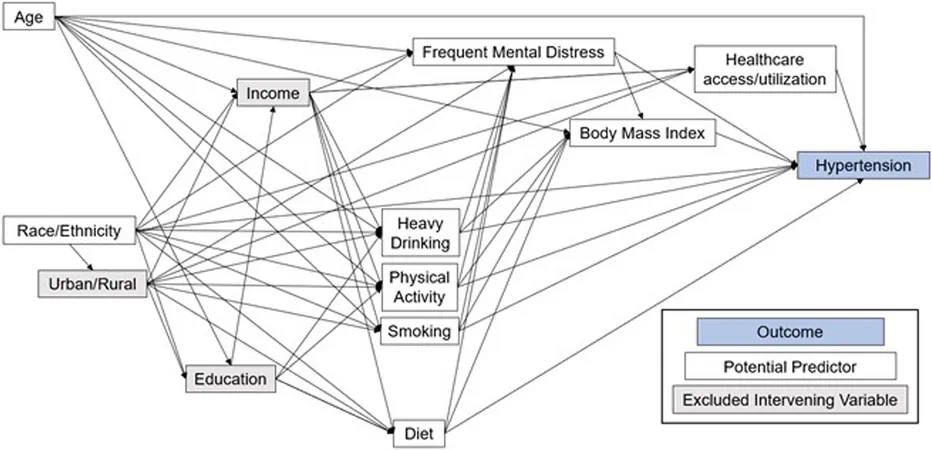
Researchers utilized data from the Behavioral Risk Factor Surveillance System (BRFSS) covering 2017, 2019, and 2021, alongside a conceptual framework to isolate potential hypertension predictors. These predictors ranged from sociodemographic factors to chronic health conditions and healthcare accessibility. Advanced statistical analysis, including binary logistic regression, was employed to pinpoint significant predictors.
Key Findings and Significant Predictors
The study unveiled alarming odds associated with hypertension: - Women experiencing frequent mental distress were **twice as likely** to report hypertension (odds ratio [OR] = 2.0). - Those living in areas with a shortage of healthcare professionals were **1.8 times more likely** - Obese women had a staggering **2.6 times higher chance** of having hypertension. - Age was also a significant factor, with women aged 35 to 44 years being **2.3 times more likely** to report high blood pressure. Interestingly, the odds were lower for women who had not seen a healthcare provider in the past year, raising questions about healthcare engagement and detection rates.
Why It Matters: The Broader Context
Chronic hypertension in women of reproductive age is concerning, as it significantly contributes to hypertensive disorders during pregnancy—one of the leading causes of maternal mortality in the U.S. The study found that rates of hypertension are climbing, partly due to rising obesity rates and higher maternal ages. North Dakota, with its vast rural landscapes and minority populations, faces unique challenges. Approximately 38 out of 53 counties are classified as primary care health professional shortage areas, leaving many women with limited access to health services. Factors such as race, socioeconomic status, and residence all play complex roles in the health disparities observed. For instance, non-Hispanic Black and American Indian women are disproportionately affected by chronic hypertension relative to their White counterparts.
Implications for Public Health
The findings highlight an urgent need for targeted public health programs in North Dakota. The emphasis should be on bolstering mental health resources, increasing healthcare access, and promoting weight management. Public health officials are encouraged to ramp up initiatives aimed at hypertension awareness, particularly in areas lacking sufficient healthcare resources. Moreover, this investigation illustrates the pressing need for further research on whether enhancing mental well-being can effectively lower hypertension risks in this vulnerable group.
Conclusion
With the prevalence of self-reported hypertension pegged at **8.9%** among women of reproductive age in North Dakota, these findings provide critical insights into the risk factors influencing this serious health issue. As hypertension rates continue to rise, understanding these predictors enables healthcare professionals to create focused strategies for better health outcomes. Policymakers and healthcare organizations must consider these findings to devise effective interventions that could save lives and improve the overall health landscape for women in reproductive age across North Dakota. The quest to combat hypertension is far from over—better awareness, prevention, and control are the keys to transforming this "silent killer" into a manageable health challenge.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)