Transforming Depression Treatment: A Groundbreaking Case Study in Pharmacogenomics
2025-01-10
Author: Arjun
Introduction
In recent years, the drive towards personalized medicine has taken root, especially in the field of psychiatry. With the escalating prevalence of non-communicable diseases (NCDs), depression stands out as a pressing mental health issue, particularly in lower-income countries. Traditional treatment approaches for antidepressants often lead to slow results and varying efficacy, prompting the need for innovative solutions. Enter pharmacogenomics—a powerful ally in the quest for tailored antidepressant therapies.
The Challenge
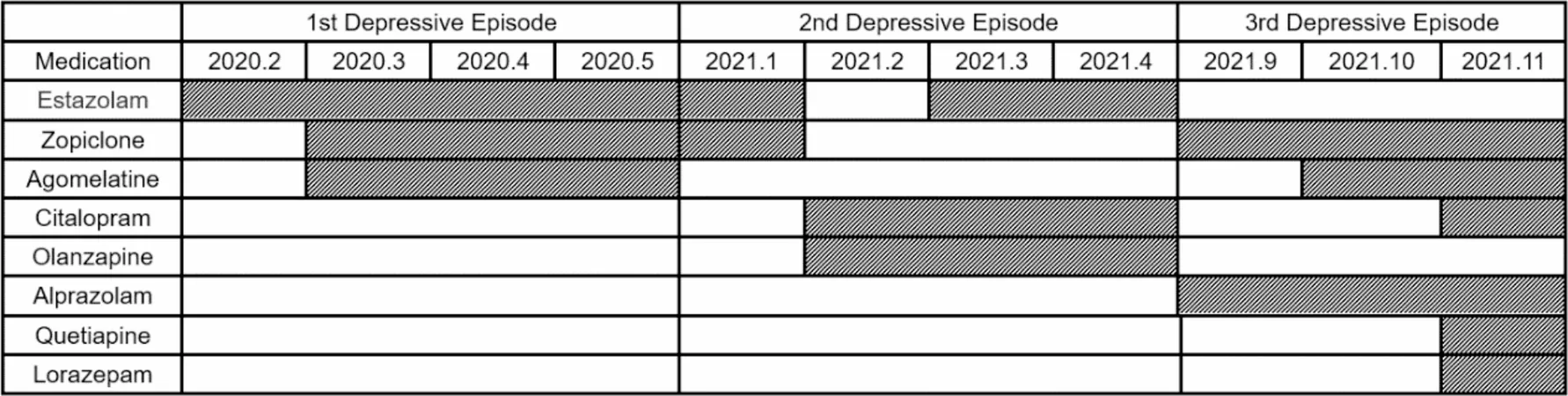
The case under review explores the journey of a 27-year-old woman battling recurrent depression. Despite multiple unsuccessful treatment attempts with conventional antidepressants, her mental health issues persisted, leading to heightened anxiety and the development of withdrawal symptoms from benzodiazepine therapy. Her plight reflects a broader trend: a staggering 50-85% recurrence rate in depression, with nearly half of patients relapsing within two years.
Breaking New Ground with Pharmacogenomics
Pharmacogenomic testing derives insights from an individual’s genetic makeup, helping clinicians tailor medication regimens more effectively. For our patient, understanding her unique genetic polymorphisms, particularly within cytochrome P450 enzymes, was crucial. These enzymes significantly influence drug metabolism, affecting both therapeutic efficacy and potential side effects. In her case, the preliminary choice of citalopram was thwarted by her intermediate metabolism of CYP 2C19, highlighting the importance of personalized approaches in tackling treatment-resistant depression.
After pharmacogenomic analysis revealed unresponsive results, clinicians pivoted towards fluvoxamine—a decision aligned with current clinical guidelines for managing major depressive disorder. This strategic shift opened the door to a marked improvement, demonstrating how targeted pharmaceutical interventions can usher in rapid symptom relief.
Current Status and Future Directions
Today, the patient shows promising signs of recovery—her depression and anxiety symptoms are better controlled, and her sleep has improved remarkably. Such outcomes underscore the pivotal role of pharmacogenomics in contemporary psychiatric care, significantly reducing the trial-and-error nature of antidepressant prescribing.
Despite its potential, there are challenges to implementing pharmacogenomic testing widely, including the limited availability of trained professionals and the cost associated with genetic testing. However, as awareness grows and more clinicians adopt these methodologies, we may witness the dawn of a new era in mental health treatment.
Conclusion
This case illuminates the promise of pharmacogenomic-guided therapy for enhancing treatment outcomes in patients with complex psychiatric disorders. By harnessing genetic insights, we can pave the way for more effective and individualized care, ultimately transforming the landscape of depression treatment. As we look to the future, it is crucial to bridge genetic findings with clinical practice, ensuring that every patient receives the care they truly need in their journey toward mental wellness.
Stay tuned for future updates as researchers continue to unravel the intricacies of pharmacogenomics in mental health—who knows what breakthroughs lie just around the corner!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)