Traditional vs. Novel β-Lactam Antibiotics for Treating Carbapenem-Resistant Pseudomonas aeruginosa: A Closer Look at Effectiveness!
2024-12-22
Author: Yu
Introduction
In the fight against antibiotic resistance, carbapenem-resistant Pseudomonas aeruginosa (CRPA) is proving to be a formidable adversary. The World Health Organization has included CRPA on its list of critical priority pathogens, highlighting the urgent need for effective treatment options. Many clinicians are left wondering whether traditional non-carbapenem β-lactams (NCBL) can compete with newer β-lactam agents (NVL) in managing CRPA infections. This retrospective cohort study digs deep into this dilemma, analyzing patient outcomes based on the antibiotic treatment received.
Study Overview
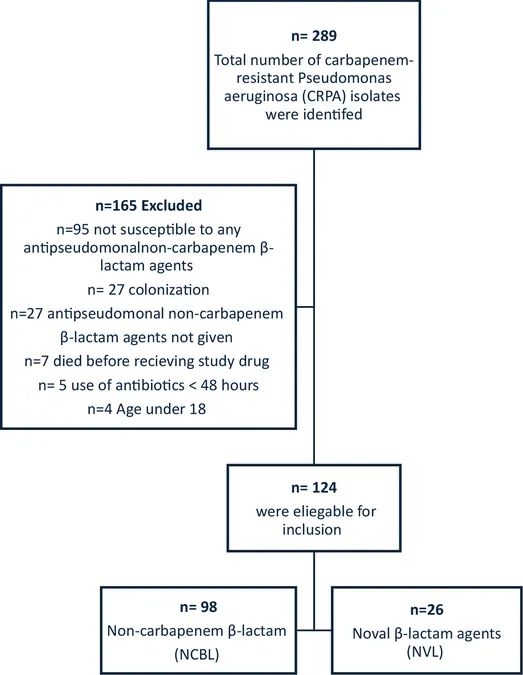
Conducted at the King Faisal Specialist Hospital in Jeddah from January 2016 to December 2022, this study involved adult patients (18 years and older) diagnosed with CRPA infections. Participants were grouped based on whether they received traditional NCBL or NVL for over 48 hours. The primary endpoint: 30-day mortality.
Key Findings
A total of 124 patients were analyzed, with about 79% receiving traditional NCBL and 20.9% receiving NVL. The initial results indicated that 30-day mortality rates were not statistically different between the NCBL (41.8%) and NVL (46.2%) groups, suggesting that both treatment pathways are similarly effective.
Of critical note, however, was the microbiological eradication rate, which was significantly higher in the NVL group (57.7% vs. 33.7% in the NCBL group), along with lower 90-day infection recurrence rates (38.5% vs. 61.2%). These findings underscore a potential advantage for NVL, sparking discussions about their use even as resistance patterns evolve.
Contextual Background
CRPA is associated with longer hospital stays and increased mortality, making effective treatment crucial. The Centers for Disease Control and Prevention has labeled multidrug-resistant P. aeruginosa a serious threat to healthcare. Traditional NCBL treatments have fallen under scrutiny, given the rise of resistance due to mechanisms like overexpression of efflux systems.
Emerging research indicates that while NVLs yield improved outcomes compared to older regimens like colistin, overutilization could provoke new resistance. The Infectious Diseases Society of America (IDSA) guidelines now suggest reverting to traditional β-lactams as effective alternatives, though comparative studies remain limited.
Clinical Implications
While the 30-day mortality rates showed no substantial difference, the increased microbiological eradication with NVL suggests that it may offer a more comprehensive treatment approach in managing CRPA. The study also highlights that critically ill patients seem to experience comparable outcomes, leading to the hypothesis that perhaps treatment choice could be reconsidered based on individual patient profiles rather than broad-spectrum guidelines.
The necessity for further research is paramount. Larger-scale studies could yield more conclusive evidence and address the limitations of this work, such as potential selection biases and varying pathogen virulence within the NCBL-susceptible cohort.
Final Thoughts
As healthcare providers continue to address the ever-evolving landscape of antibiotic resistance, the outcomes of using traditional versus novel β-lactams in CRPA treatment necessitate further examination. With a disease known to elevate hospital stays and mortality rates, understanding the effectiveness and intricacies of these antibiotics could inform better treatment practices and ultimately save lives.
This study stands as a significant contribution to the field, emphasizing that while both NCBL and NVL treatments are viable, the higher microbiological success rates of NVL merit further exploration and application in clinical settings for optimal patient outcomes. The stakes are high, and the fight against CRPA is far from over!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)