The Unseen Connection: How Heart Failure Increases the Risk of Diabetes and What You Can Do About It
2024-09-28
Author: Nur
Diabetes and heart failure (HF) are more than just two chronic conditions; they are interlinked in a bidirectional relationship that can significantly worsen health outcomes. Individuals with diabetes face a heightened risk of developing heart failure across all glucose levels, while those suffering from heart failure are equally vulnerable to developing diabetes. This alarming synergy calls for an urgent need to detect glucose abnormalities to prevent diabetes among heart failure patients.
Heart Failure and Diabetes: A Dangerous Link
Research indicates that the presence of diabetes not only amplifies the risk of heart failure but also complicates the prognosis for those already diagnosed with heart failure. Approximately 42% of patients with heart failure with reduced ejection fraction (HFrEF) and 45% of those with heart failure with preserved ejection fraction (HFpEF) also battle diabetes. Disturbingly, this incidence has been on the rise over the past 15 years. Diabetic patients have more than double the chance of developing heart failure compared to non-diabetic individuals—a risk that extends even after adjusting for age and other comorbidities. Studies have shown that diabetes can increase the risk of heart failure twofold for men and up to fivefold for women.
The danger is particularly pronounced among younger patients or those experiencing recent-onset diabetes. Essential risk factors include age, obesity, and existing cardiovascular conditions such as coronary artery disease. In fact, heart failure may manifest as one of the first signs of cardiovascular complications in diabetes patients, often without prior signs of heart disease.
The Alarming Rise of Diabetic Cardiomyopathy
Diabetic cardiomyopathy is a serious condition characterized by changes in the heart's structure and function due to chronic high blood sugar levels. It manifests as both systolic and diastolic dysfunction, demonstrating that the harmful effects of diabetes on the heart are substantial. Furthermore, the presence of obesity, hypertension, and chronic kidney disease tends to compound these problems, resulting in deteriorating heart function.
Recent molecular studies have pointed to the involvement of unique proteins and pathways, such as the JunD/PPAR-γ mechanism, which contribute to heart dysfunction in diabetes patients. Elevated levels of specific lipids in the heart have also been associated with increased risks of developing heart failure.
A Two-Way Street: How Heart Failure Contributes to Diabetes Development
What’s equally concerning is that heart failure doesn't just raise the risk of diabetes; it can act as a catalyst, leading to newly diagnosed diabetes. Patients with heart failure often experience insulin resistance, which can complicate glucose management. Notably, in individuals with a higher body mass index and other cardiovascular risk factors, the likelihood of transitioning to diabetes increases significantly.
For example, a study involving older adults demonstrated that those with heart failure developed prediabetes at nearly twice the rate of those without. The need for regular monitoring and intervention becomes paramount.
The Silent Epidemic of Undiagnosed Dysglycemia
Undiagnosed diabetes and prediabetes are rampant among heart failure patients. A lack of routine glucose screening, often compounded by misdiagnosis, further exacerbates this issue. Patients typically miss out on necessary interventions until their condition significantly deteriorates.
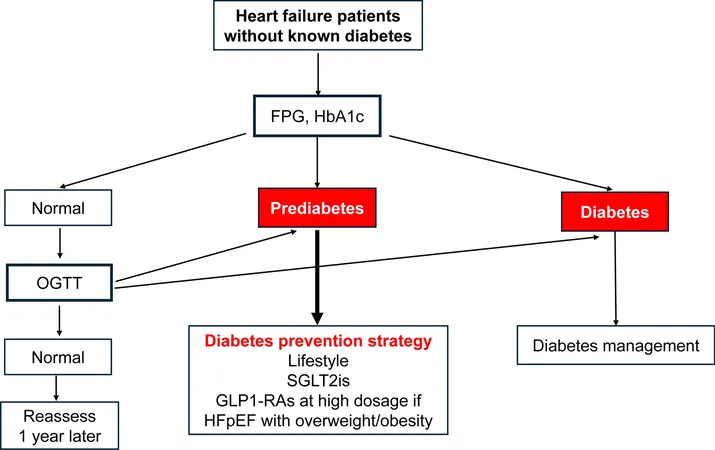
The oral glucose tolerance test (OGTT) remains the gold standard for early detection of diabetes and undiagnosed dysglycemia. Studies have shown that using only fasting blood glucose measurements may lead to underdiagnosis, as many patients fall into the prediabetic or undiagnosed diabetic categories.
Prevention is Key: Early Detection and Intervention
Preventive strategies are critical for managing both heart failure and diabetes. For patients exhibiting risk factors such as obesity or hypertension, regular glucose screenings should be a routine part of care. Lifestyle interventions, effective at reducing the risk of diabetes among those with prediabetes, must be emphasized. Studies show that even modest weight loss can significantly mitigate risks, potentially preventing diabetes at the prediabetic stage.
Incorporating glucose-lowering interventions, especially SGLT2 inhibitors and GLP-1 receptor agonists, has shown promise in protecting against the development of diabetes while managing heart failure symptoms. Clinicians should adopt a proactive approach, advocating for lifestyle changes alongside medical treatments aimed at improving glycemic control.
Conclusion: A Call to Action
The intersection between diabetes and heart failure represents a pressing health challenge that needs immediate attention. As healthcare professionals, we must prioritize screening and monitoring of metabolic status in heart failure patients. Knowledge is power, and the time is now to implement strategies that could prevent patients from spiraling into a cycle of worsening health conditions.
Stay informed, mobilize your care team, and advocate for change. Together, we can tackle this silent epidemic before it claims more lives.
If you or someone you know is at risk, don’t wait for symptoms to appear—contact your healthcare provider today for a check-up!





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)