The Sleep-Depression Link in Older Adults: Shocking Study Findings You Need to Know!
2025-01-24
Author: Daniel
Introduction:
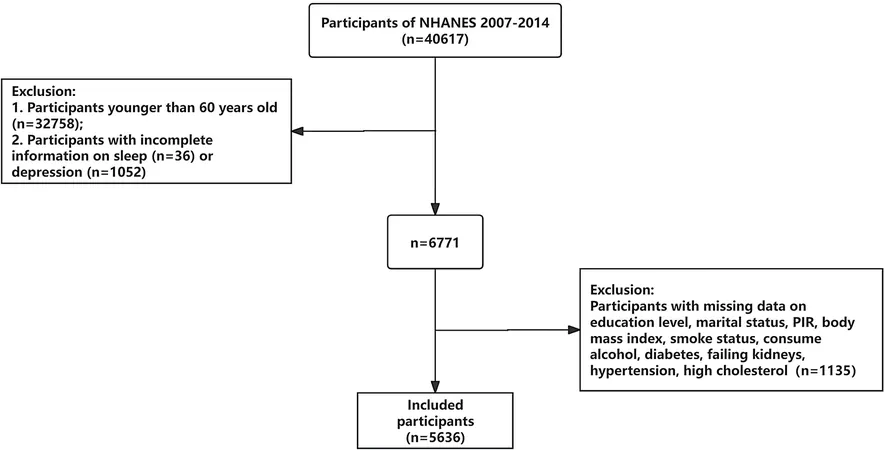
A groundbreaking cross-sectional study has revealed a startling connection between sleep patterns and depression in older adults based on data from the National Health and Nutrition Examination Survey (NHANES) conducted between 2007 and 2014. With the global geriatric population projected to reach 2 billion by 2050, understanding this relationship is more crucial than ever.
Study Overview:
The aim of the study was to investigate how various sleep behaviors, including sleep duration and sleep disorders, correlate with the risk of depressive symptoms in individuals aged 60 and older. A robust dataset comprising 5,636 participants was analyzed, unveiling some eye-opening statistics about sleep and mental health.
Findings:
The research reported an overall depression prevalence of 7.7%. Alarmingly, this figure was significantly higher among older women, whose depression rate was 1.6 times more than that of older men. The study classified sleep patterns into healthy, intermediate, and poor categories. It was found that older adults with intermediate sleep patterns had twice the risk of depression compared to those with healthy sleep. Even more troubling, those with poor sleep patterns faced shocking 5.6 times higher odds of experiencing depression.
Participants who slept less than 7 hours per night were found to have 2.04 times higher prevalence of depression, while those without sleep issues showed a drastically reduced rate, underscoring the importance of quality rest.
Significance of Sleep Disorders:
As the percentage of older adults seeking care for depression continues to rise, it's clear that sleep disorders play a substantial role. For instance, conditions like obstructive sleep apnea can lead to increased cardiovascular risks, cognitive decline, and mood disturbances.
Sleep disorders are particularly rampant among older adults: studies indicate that approximately 35.9% of older Chinese adults reported sleep problems, a pattern that is likely replicated across the globe. This pervasive issue emphasizes the need for targeted interventions to improve sleep quality and subsequently mental health outcomes.
Implications for Mental Health:
Given the high stakes of untreated depression, including difficulties with treatment adherence and increased hospitalization, addressing sleep issues among older individuals can offer a vital pathway to enhance quality of life. Mental health professionals must screen for sleep disorders in older patients exhibiting depressive symptoms, as tackling sleep issues could significantly alleviate depressive disorders.
Cultural and Global Context:
Globally, different cultural attitudes towards aging and mental health can influence the presentation and acknowledgment of depression in older adults. For example, studies from countries like Vietnam have shown staggering self-reported depression rates among the elderly. Such findings reinforce the idea that while sleep and depression are critical aspects of health, cultural context plays a significant role in how these problems manifest and are treated.
Conclusion:
This study's revelations highlight an urgent need: recognizing the relationship between sleep patterns and depression in the elderly is not just an academic exercise—it's a public health imperative. As we move forward, ongoing research must seek to understand the intricate mechanisms at play, paving the way for better mental health strategies for older populations around the world.
Stay Awake to the Dangers of Poor Sleep!
If you or someone you know is experiencing sleep problems or depression, don’t wait—seek help today!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)