The Hidden Shield: How Melanoma Outsmarts Immunotherapy and What It Means for Patients
2025-03-28
Author: Wei
Cutaneous melanoma, the most aggressive form of skin cancer, is notorious for its ability to evade the immune system, despite its high mutation load. Shockingly, more than half of patients undergoing current immunotherapies see little to no benefit. This alarming reality raises crucial questions about the mechanisms tumors employ to hide and resist treatment.
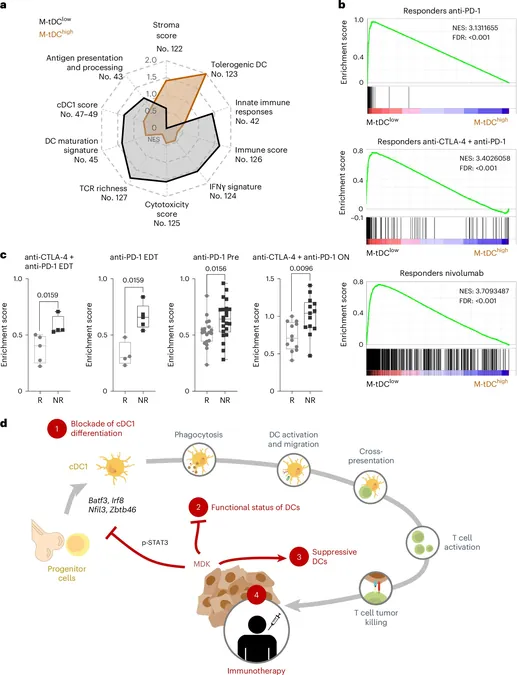
In a groundbreaking study published in Nature Cancer led by Marisol Soengas of the Melanoma Group at the National Cancer Research Center (CNIO), researchers uncovered a clever tactic utilized by melanomas and other aggressive tumors. The study reveals that melanoma cells secrete a protein called Midkine that decreases the presence of dendritic cells, crucial immune defenders that recognize and attack tumors. Dendritic cells function as the immune system's sentinels, presenting tumor antigens to cytotoxic T lymphocytes, which are essential for controlling and eliminating malignancies. However, melanoma's manipulation of Midkine not only reduces the number of these sentinel cells but also reprograms them to favor tumor growth instead of fostering an immune response.
"Midkine acts as both a shield and an accelerator for tumors," explains Soengas. This dual role complicates matters severely—by suppressing immune recognition and boosting malignant spread, melanoma demonstrates remarkable resilience against traditional therapies.
When investigating the potential effects of this mechanism on immunotherapy treatments, the CNIO research team found promising results in animal models. Inhibiting Midkine not only enhanced the efficacy of dendritic cell-targeting vaccines but also improved the performance of immune checkpoint inhibitors, a widely used class of immunotherapy.
This revelation opens the door to the development of new therapeutic strategies aimed at counteracting the immunosuppressive effects of Midkine. The researchers also analyzed large patient cohorts and identified a specific gene signature associated with Midkine activity in dendritic cells, which correlates with a poor prognosis across various cancers, including lung, breast, endometrial, adrenal gland, and mesothelioma cancers.
These findings emphasize the urgent need for innovative therapies that can reactivate dendritic cells and overcome the immunosuppressive benefits that Midkine affords aggressive tumors.
As we continue to unravel the intricate mechanisms that allow melanoma and other cancers to persist and thrive, this research represents a critical step toward more effective treatments. The battle against melanoma is not over yet, and understanding the secrets of its survival is imperative for improving patient outcomes and advancing the field of oncology.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)