The Hidden Link Between Early Menopause and Worsening Rheumatoid Arthritis Symptoms
2025-03-24
Author: Wei
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that predominantly affects women, often leading to severe and irreversible joint damage, disability, and increased risk of mortality. The menopausal transition is a critical phase in a woman's life marked by reduced estrogen levels, which significantly impact various aspects of health, including bone density, cardiovascular health, and the risk of neurodegenerative issues. Moreover, this transition can lead to bothersome symptoms such as hot flashes and mood swings, ultimately affecting the quality of life.
Research has shown a notable connection between the onset of RA and the stages of menopause. The peak onset of RA in women often aligns with menopausal years, prompting researchers to explore whether menopause could influence the severity and characteristics of the disease. Interestingly, early menopause (EM), defined as the onset of menopause before age 45, has been identified as a risk factor for the development of RA.
Recent studies indicate that women undergoing early menopause exhibit a staggering 2.4 times higher risk of developing RA compared to their peers experiencing menopause at a later age. Patients with EM often face a unique set of challenges, including a higher prevalence of somatoform autonomic dysfunction, possibly leading to amplified pain perception and negatively impacting disease outcomes.
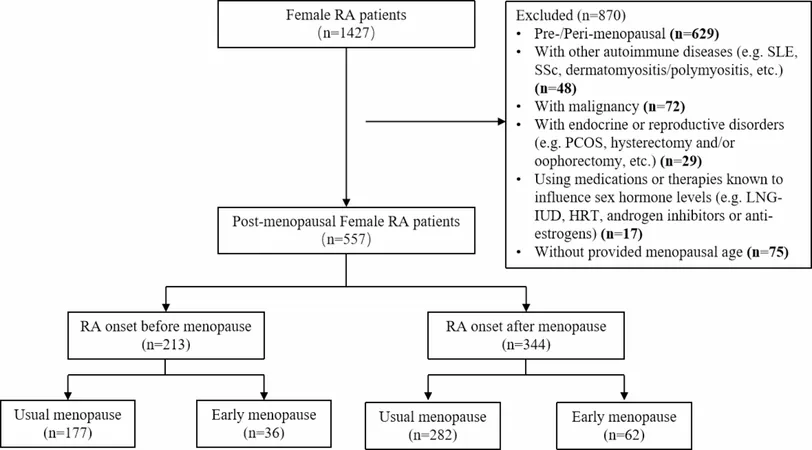
In an extensive observational study with over 1,400 female RA patients, researchers sought to clarify the temporal relationship between RA onset and menopause, while specifically examining the impact of early menopause on disease activity. The findings revealed that women with EM reported higher levels of disease activity and poorer patient-reported outcomes (PROs) when compared to those with usual menopause (UM), particularly in those whose RA began after menopause. The presence of a longer disease duration and more severe symptoms like pain and disability were particularly pronounced in these women.
A striking correlation emerged: even after adjusting for confounding factors such as age and disease severity, early menopause remained a significant predictor of worse disease outcomes in RA patients. This suggests that the effects of EM extend beyond mere inflammation, hinting at the role of central sensitization—the process by which the nervous system becomes sensitized to pain.
It's crucial to understand that while EM is relatively common among women, its prevalence is particularly high among those with autoimmune conditions. For instance, studies show that the occurrence of EM in patients with systemic diseases can be as high as 44%. The reasons behind this phenomenon remain elusive but may include autoimmune disorders and other underlying health issues.
Given these findings, healthcare professionals must consider the implications of early menopause when devising treatment plans for RA patients. Tailored approaches, rather than solely aggressive anti-inflammatory treatments, may offer better outcomes, specifically through addressing both inflammatory and non-inflammatory disease aspects. Potential strategies could include hormone replacement therapy or pain management programs that target central sensitization.
Ultimately, the intersection of early menopause and rheumatoid arthritis reveals a complex relationship that warrants further investigation. By understanding this link, clinicians may be better equipped to support women through this challenging phase of life—enhancing their quality of life and potentially mitigating the severity of rheumatoid arthritis symptoms.
Stay informed and proactive about the hidden impacts of menopause on autoimmune health; your journey to better health could depend on it!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)