The Hidden Link Between Arthritis and Depression: What Recent Findings Reveal
2024-11-05
Author: Li
Arthritis, a prevalent chronic condition that affects millions globally, particularly impacts middle-aged and older individuals. This common ailment, characterized by pain and disability, not only restricts mobility but can also lead to significant emotional distress. Recent research has illuminated the intricate relationship between arthritis and depressive symptoms, revealing that mental health plays a pivotal role in the progression and management of this debilitating condition.
A staggering 154.4 million older adults in China alone are afflicted by arthritis, representing 31.4% of this demographic. Globally, over 55% of those living with arthritis are older than 55 years, highlighting the urgent need for effective interventions as populations age. Patients with arthritis often report severe fatigue, limited activity, and emotional turmoil, with the pain of arthritis frequently exacerbating depressive symptoms.
According to the 2022 World Mental Health Report from the World Health Organization (WHO), around 1 in 8 individuals worldwide are affected by mental health disorders, with depression being a primary concern. In China, depression impacts approximately 30-43% of individuals over 45 years, indicating a concerning trend among those grappling with both arthritis and mental health issues. Studies have shown that individuals experiencing depressive symptoms may suffer significantly poorer health outcomes and quality of life, leading to a vicious cycle that worsens both mental and physical health.
Traditionally, studies have indicated that individuals with arthritis are at an elevated risk for developing depression. However, emerging research suggests that the reverse may also hold true—depression could significantly increase the likelihood of developing arthritis. One notable study from Taiwan provides substantial evidence of a bidirectional relationship, showcasing that worsening depressive symptoms can lead to a greater risk of rheumatoid arthritis (RA). This association may be related to underlying inflammatory processes linked to both depression and arthritis.
Despite these findings, the relationship remains complex and sometimes contradictory. Some community surveys have failed to establish a clear connection, suggesting that factors such as race, geographical differences, and study demographics may contribute to the variability in outcomes. Consequently, there is a pressing need for ongoing research to clarify how changes in depressive symptoms over time impact the development and progression of arthritis.
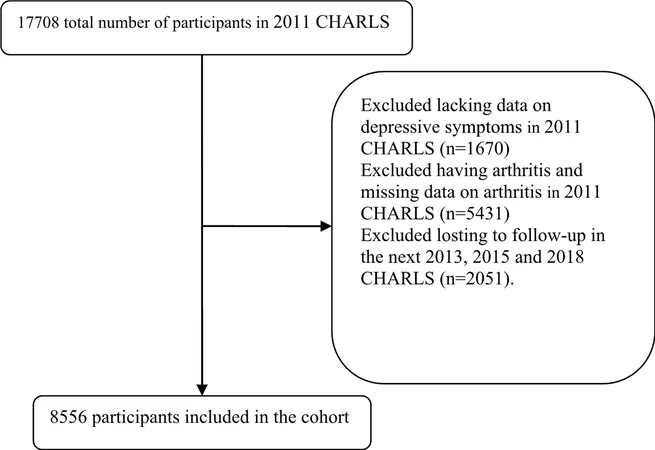
In a recent longitudinal study utilizing data from the China Health and Retirement Longitudinal Study (CHARLS), researchers sought to investigate how fluctuations in depressive symptoms correlate with arthritis incidence in older adults. They hypothesized that worsening mental health would correlate with increased arthritis risk, while improvements might reduce it. The findings confirmed that those whose depressive symptoms improved were 25% less likely to develop arthritis, while new cases of depression increased the likelihood of arthritis by 66%.
Using the CES-D-10 scale, researchers assessed depressive symptoms, and self-reports determined the presence of arthritis. Among the 8556 participants studied, it was evident that depressive symptoms significantly influenced the risk of developing arthritis, with a 1-point increase in depressive scores correlating to a 4-5% increase in arthritis risk after an 8-year follow-up.
Further analyzing factors such as age, sex, marital status, and lifestyle choices revealed that the association between depression and arthritis remained consistent across demographic groups. Notably, it was found that unhealthy behaviors often associated with depression, such as smoking and a sedentary lifestyle, likely exacerbate arthritis symptoms, creating a feedback loop that complicates treatment and recovery.
The implications of these findings are profound. Healthcare providers must prioritize mental health screenings for individuals with arthritis, as depression can significantly hinder treatment outcomes and overall quality of life. Furthermore, strategies aimed at improving mental health could be an effective adjunct to arthritis management, potentially mitigating the physical consequences of both conditions.
Despite the strengths of this extensive study, including its large sample size and prospective design, it does have limitations. For instance, self-reported data may lead to discrepancies in accuracy, and the lack of differentiation between types of arthritis could impact the generalizability of the findings. Nevertheless, the evidence presented emphasizes a crucial link between mental health and physical well-being, advising health professionals to adopt a more holistic approach when treating patients with arthritis.
In conclusion, the complex interplay between arthritis and depressive symptoms calls for increased awareness and targeted strategies. As the prevalence of arthritis continues to rise in an aging population, understanding how mental health influences the trajectory of physical conditions like arthritis could pave the way for innovative treatments and better patient care.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)