The Hidden Dangers of Polypharmacy Among Elderly Psychiatric Patients: Unpacking Anticholinergic Burden
2025-01-20
Author: Yu
As the global population ages, mental health disorders are becoming increasingly prevalent among older adults, especially those aged 60 and above. According to the Global Burden of Disease Study 2019, about 21.4% of this demographic faces some form of mental health issue. Conditions such as depression, anxiety, and cognitive impairment can lead to significant distress and impair everyday functioning. Unfortunately, the medications designed to alleviate these symptoms can sometimes do more harm than good.
What is Anticholinergic Burden?
A hidden threat in the realm of medication management for the elderly is what's called "anticholinergic burden." Anticholinergic drugs, commonly used for a variety of conditions (from Parkinson's to allergies), can have significant side effects, particularly on cognitive functioning. This burden accumulates when a patient is on multiple medications—known as polypharmacy—which is especially common among older adults. Alarmingly, studies reveal that between 20 to 40% of those over 60 are prescribed five or more medicines concurrently.
Anticholinergic Medications: A Double-Edged Sword
Anticholinergic medications can often be found in psychotropic treatments such as antidepressants, anxiolytics, and antipsychotics. Research indicates that cognitive decline in older adults may not simply be attributed to age but also to these medications' anticholinergic effects. The risk compounds when patients take multiple medications with anticholinergic properties, potentially leading to severe cognitive impairments, memory issues, increased likelihood of falls, and even higher mortality rates.
Assessing the Anticholinergic Burden: The Tools of the Trade
Several scales have emerged to measure anticholinergic burden, each with various methodologies. The well-regarded Anticholinergic Cognitive Burden (ACB) Scale ranks medications based on their impact on cognition. The Anticholinergic Risk Scale (ARS) and the Anticholinergic Drug Scale (ADS) are also used to categorize drugs based on their anticholinergic potential.
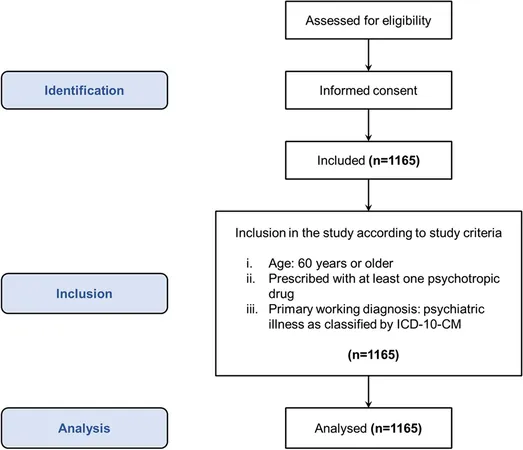
In a recent cross-sectional study conducted at the All-India Institute of Medical Sciences (AIIMS) in Rishikesh, researchers sought to examine the extent of polypharmacy and its related anticholinergic burden among elderly psychiatric patients. This study adhered to rigorous ethical standards and included over a thousand patients aged 60 and above, providing a significant sample for statistical evaluation.
Key Findings and Insights: A Reality Check
Among the 1,165 participants, more than 20% were classified as experiencing polypharmacy, with the highest rates occurring in patients aged 75 and older. Notably, clonazepam and escitalopram were among the commonly prescribed anticholinergic drugs, with patients often showing severe adverse drug reactions like sleep disturbances and tremors.
The study highlighted that men generally faced higher levels of polypharmacy across various age groups, although women aged 65-69 had higher rates than their male counterparts. Key disorders identified included major depressive disorder and anxiety disorders, underscoring the link between mental health conditions and medication use.
A Call to Action: Stop the Cycle of Harm
To mitigate the risks associated with polypharmacy and anticholinergic burden, healthcare professionals must carefully evaluate patient medication regimens. Efforts aimed at reducing unnecessary medications should be a priority to prevent cognitive decline and enhance quality of life for older adults. By carefully monitoring medications' effects and employing the available anticholinergic burden scales, practitioners can better safeguard the health of their elderly patients.
Conclusion: A Growing Concern
The findings from this study underscore a critical healthcare issue: the potential dangers posed by polypharmacy and anticholinergic burden in older adults. As our population ages, it is imperative for medical practitioners, caregivers, and patients themselves to remain vigilant in managing healthcare strategies effectively. This could involve saving lives and preserving cognitive function for many elderly individuals grappling with mental health issues.
With the prevalence of polypharmacy only expected to rise, understanding and addressing its implications is not just advisable—it's essential for the well-being of our aging population.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)