The Hidden Danger: How Sleep Apnea Severity Links to Cognitive Decline
2025-08-15
Author: Daniel
Obstructive Sleep Apnea (OSA) is more than just a sleep disorder—it's a global health crisis affecting around 1 billion people aged 30 to 65. This condition disrupts breathing during sleep, leading to complications like daytime drowsiness, cardiovascular issues, and alarmingly, cognitive impairment.
Recent studies estimate that 37-48% of individuals with OSA suffer from Mild Cognitive Impairment (MCI), a crucial yet often overlooked cognitive syndrome that sits precariously between normal aging and full-blown dementia. As scientists dive deeper into the connection between sleep disturbances and cognitive health, they’re unraveling compelling links that could change the clinical approach to managing OSA.
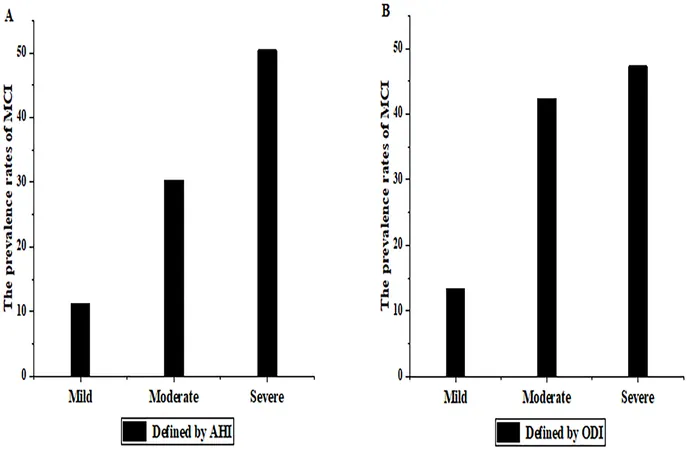
One major revelation is that people with OSA face a 26% increased risk of cognitive decline. But how does the severity of their sleep apnea play into this? Current research points to an intriguing correlation: those suffering moderate to severe OSA often show higher incidences of MCI.
Controversy Surrounding Diagnosis
Despite promising correlations, the relationship between OSA and MCI generates debate. Variations in study designs, MCI diagnostic tools like the Montreal Cognitive Assessment (MOCA), and differing definitions of OSA create a complex landscape. Using MOCA, researchers hope to gain clearer insights into the cognitive issues tied to sleep apnea.
Excessive Daytime Sleepiness (EDS) is another common symptom of OSA, often reported as an uncontrollable urge to sleep during the day. This drowsiness complicates everyday tasks and can lead to dangerous situations like impaired driving. Yet, its direct link to cognitive decline remains underexplored.
Research Objectives and Methodology
To bridge these gaps, a study at Jinzhou Medical University sought to evaluate the prevalence of MCI in OSA patients while assessing the influence of sleep apnea severity on cognitive function. Encompassing over 387 participants, the study employed thorough assessments, including sleep studies using polysomnography (PSG) and cognitive tests using MOCA.
Participants were categorized based on their OSA severity, directly linking it to MCI risk. The study’s findings promise to reshape early diagnostic strategies and treatment plans for cognitive issues among OSA patients.
The Alarming Results
The results revealed staggering statistics: the prevalence of MCI was highest among participants with severe OSA, at 50.4%. This rate dramatically dropped to just 11.2% for those with mild OSA. This indicates a clear trend: the more severe the OSA, the greater the risk of cognitive impairment.
Exploring Other Influencing Factors
The study doesn't stop there—it also addresses the impact of EDS and sleep quality on cognitive health. Adjusted analyses found that poor sleep quality and heightened daytime sleepiness significantly raised the risk of MCI. These insights underscore the critical need for improving sleep conditions to mitigate cognitive decline among OSA sufferers.
Recommendations for Clinicians
The findings highlight that treating sleep apnea effectively might not only reduce symptoms but could also stave off cognitive decline. Clinicians are urged to prioritize early interventions for OSA, including Continuous Positive Airway Pressure (CPAP) therapy, which has shown promise in reversing cognitive deficits.
While the study does have its limitations, including a lack of control groups and reliance on MOCA for diagnosing MCI, it opens the door for further research into comprehensive cognitive assessments. With the rising prevalence of OSA, understanding its implications on cognitive health is more crucial than ever.
A Wake-Up Call for Everyone
For individuals suffering from sleep apnea or experiencing symptoms of daytime drowsiness, this research serves as a wake-up call. The implications of untreated OSA extend beyond just sleepy days; they could reshape cognitive futures. Addressing sleep health isn't merely about better rest—it could be the key to preserving mental acuity as we age. The stakes have never been higher!
Conclusion
As we stand on the brink of understanding the intricate dance between sleep and cognition, raising awareness about OSA and its neurological effects is essential. Those with sleep apnea should not only seek treatment for better nights but also for sharper days.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)