The Hidden Crisis: Contraceptive Access and Use Among Migrant Women in Wealthy Nations - What You Need to Know!
2024-09-20
In the face of increasing global migration fraught with socio-political turmoil, economic instability, and climate change, the issue of sexual and reproductive health and rights (SRHR) has emerged as a pressing concern, especially for women with migratory experiences. The Guttmacher-Lancet Commission articulated SRHR as a fundamental state of well-being encompassing physical, mental, and social health, affirming the right of all individuals to govern their bodies and access necessary services.
An alarming trend is revealed through statistics from the International Organization for Migration, which noted that in 2020, 281 million international migrants, including over 30 million refugees and asylum seekers, have made high-income countries their home, with women comprising nearly half of this population. Despite this, migrant women encounter unique barriers that hinder their access to crucial health services, particularly in terms of sexual and reproductive healthcare and contraceptive use. Indeed, many studies indicate that migrant women experience higher maternal mortality rates and unintended pregnancies compared to local populations.
Research consistently demonstrates a significant unmet need for contraception among migrant women living in affluent countries. For instance, a study conducted on refugee women in Canada uncovered that nearly one-third were not utilizing any form of contraception, while foreign-born women in Finland showed double the odds of contraceptive non-use compared to their Finnish-born counterparts. This trend is echoed in Sweden, where immigrant women reported decreased familiarity and usage of contraceptive methods, leading to elevated rates of induced abortion.
Despite prior descriptive studies emphasizing contraceptive prevalence and comparisons with majority populations, there is a notable shortfall in understanding the determinants of contraceptive access among migrant women in high-income contexts. To address this gap, a comprehensive scoping review synthesizes existing literature on the access and utilization of contraceptive services among women with migration experiences, shedding light on geographic areas prevalent with such populations, namely Europe, North America, and Australasia.
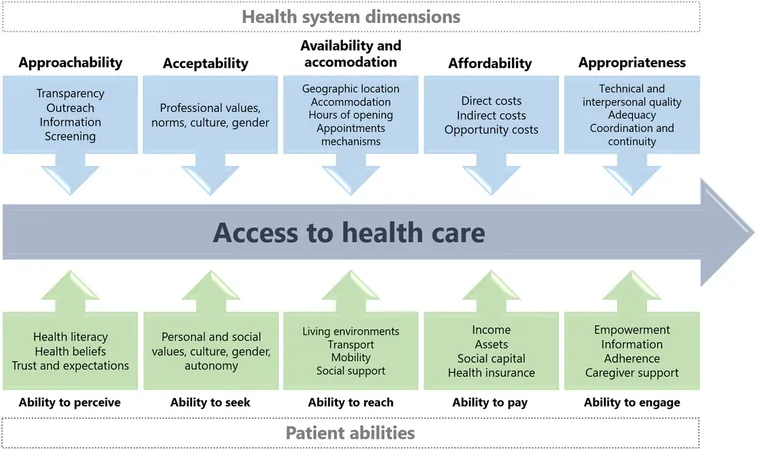
The analytic framework adopted for this review is grounded in Levesque et al.’s model regarding healthcare access, which categorizes two pivotal dimensions: the health system (supply-side) and the patient (demand-side). With regard to healthcare accessibility, both aspects are intrinsically linked and shape women’s experiences when seeking contraceptive services. Various barriers have been illuminated, including limited information about available contraceptive services, concerns about cultural acceptability, affordability, and discrimination faced during healthcare interactions.
Key barriers that emerged include:
1. Limited Information and Awareness: A significant number of women lacked awareness about where and how to access contraceptive services. Many expressed a scarcity of credible information regarding different contraceptive methods and their respective side effects, reinforcing the need for targeted educational initiatives.
2. Cultural and Religious Influences: Cultural beliefs and religious practices often shape women's attitudes toward contraceptive use. In some cases, healthcare providers failed to recognize and address these influences, resulting in a disconnect between service provisions and patient needs.
3. Language Barriers: A persistent issue highlighted was the challenge of language proficiency, which could hinder effective communication during contraceptive counseling sessions. This emphasizes the critical necessity of culturally competent healthcare providers and interpreters to enhance understanding and build trust.
4. Affordability Concerns: Cost remains a central constraint for many women. Several studies indicated that the financial burden related to contraceptives was a disincentive to using them, particularly among low-income migrant populations.
5. Discrimination in Healthcare Settings: Encounters with biased or discriminatory attitudes from healthcare providers led to feelings of mistrust and reluctance to seek necessary contraceptive services, accentuating the need for sensitivity training among practitioners.
In light of these findings, the review calls for urgent action to address individual and systemic barriers to contraceptive access for migrant women. It emphasizes the necessity for inclusion of women’s perspectives in the design of policies and health service provisions that meet their unique needs. This concentrated effort can mitigate the compounded vulnerabilities of migrant women and improve their overall reproductive health outcomes.
As we face the challenges posed by burgeoning international migration, prioritizing equitable access to contraceptive health services is not merely a matter of social justice—it's a critical step toward safeguarding the health and well-being of all women. You can be part of this change! Advocate for accessible healthcare solutions today!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)