The Hidden Battle Against Hepatitis C: How Injecting Partnerships Can Drive Change
2025-05-08
Author: Jia
In an alarming twist, despite groundbreaking advancements in hepatitis C virus (HCV) treatments over the past three decades, the epidemic is far from over. Today, around 2.1 to 4.7 million people in the U.S. are living with chronic HCV, making it a persistent threat to public health.
Before the onset of the COVID-19 pandemic, HCV was the leading infectious disease killer in the U.S., with a staggering mortality rate of 4.13 deaths per 100,000 person-years between 2016 and 2017. But that's not all—recent data reveals that HCV cases have more than doubled from 2014 to 2020, with a concerning 7% increase from 2020 to 2021. Alarmingly, people who inject drugs (PWID) represent the bulk of these new infections, with HCV prevalence rates soaring as high as 90% in this group.
Understanding the Transmission Pathways
HCV spreads primarily through sharing injecting equipment. Among PWID, infection is often a dangerous dance within injecting partnerships—individuals who regularly share needles and syringes. A critical hurdle in managing this epidemic is the lack of awareness regarding HCV, compounded by a complex two-step diagnostic process. This process begins with a quick fingerstick test but requires a follow-up venipuncture test for accurate diagnosis.
Moreover, some individuals can clear the infection spontaneously, making it essential for partners to keep up with regular testing to accurately report their health status. This research aims to shed light on how HCV status disclosure affects prevention efforts and the behaviors that can mitigate the spread within injecting partnerships.
The Power of Communication
Interpersonal communication among PWID networks is crucial for elevating HCV awareness and facilitating access to healthcare. However, research on HCV status disclosure between these injecting partners remains surprisingly scarce. One study highlighted alarmingly low rates of disclosure among rural PWID, emphasizing the critical need for interventions that encourage sharing of HCV status to prevent further transmission.
Understanding each other's HCV status aids both partners in making safer choices and prompts them to initiate testing regularly. This kind of open communication also transforms injecting partners into vital support systems for managing HCV symptoms and adhering to treatment protocols.
Investigating Disclosure Patterns
This study dives into HCV status disclosure among injecting partnerships to uncover the patterns based on their respective statuses. By analyzing self-reported data from PWID and their partners in urban environments like San Francisco and Montreal, we aimed to reveal the extent of HCV disclosure and its implications.
The Partner Study: A Closer Look
Employing a well-structured study, we gathered baseline data from drug use and HCV prevalence among injecting partnerships between 2016 and 2019. This involved rigorous eligibility assessments and behavioral surveys administered to both partners, ensuring that their participation was informed and voluntary.
Key Findings: Trends in HCV Disclosure
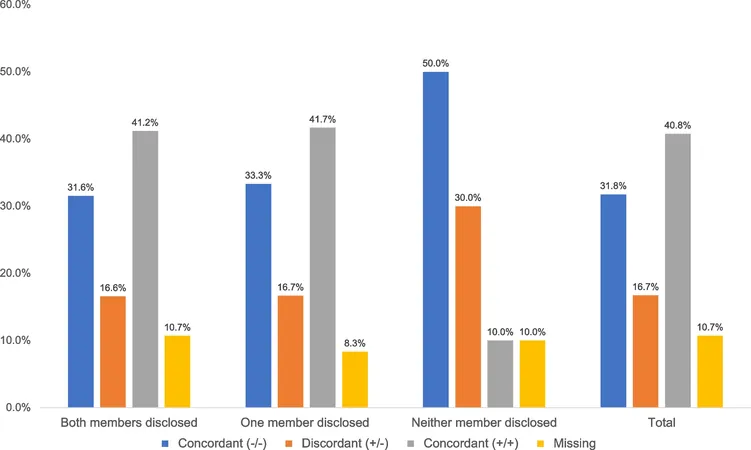
Our findings astonishingly indicate that among 179 participants, 91% reported having been tested for HCV. Furthermore, mutual disclosure of HCV status was present in 79% of partnerships, showcasing the effectiveness of open communication within these relationships. However, discordant partnerships exhibited lower disclosure rates, highlighting disparities that need addressing.
The Requests for Change
These insights underline the need for innovative public health strategies, particularly in enhancing HCV testing and disclosure practices among PWID. As evidenced by our data, higher rates of sharing HCV status correlate with safer injecting practices, thus offering a strategic avenue for reducing transmission rates within this vulnerable group.
Bridging the Gap in HCV Awareness and Care
This study not only sheds light on the dynamics of HCV transmission but also emphasizes the crucial role interpersonal relationships play in health awareness. Public health campaigns should leverage this insight to foster environments where PWID feel safe and supported in disclosing their health statuses without fear of stigma.
We must blur the lines between stigma and healthcare access, empowering individuals to take charge of their health while enhancing community efforts towards harm reduction. By fostering dialogue, we can identify barriers to disclosure and implement effective education strategies. Therefore, the street-level realization of shared responsibility in combating HCV opens the door to improved health outcomes for all.
Conclusion: Empowering Change Through Knowledge
In conclusion, this research highlights the urgent need for educational initiatives and supportive services that encourage HCV status disclosure amongst PWID. Focusing on building trusting relationships and reliable testing methods, we can create a pathway to more effective prevention and treatment strategies—one partnership at a time.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)