The Groundbreaking Crispr Treatment: A Hopeful Yet Slow Journey for Patients with Sickle Cell Disease
2024-12-23
Author: Sarah
Introduction
Deshawn “DJ” Chow, a 19-year-old from Los Angeles, has faced the agonizing reality of sickle cell disease since birth. This inherited blood disorder causes his red blood cells to take on a crescent shape, leading to painful blockages in blood flow and severe pain crises that have often confined him to the hospital. Approximately 100,000 individuals in the U.S., predominantly Black, share his struggle.
The Casgevy Treatment
Despite the persistent pain that impacted his high school experience—including missed classes and social events—Chow discovered a potential breakthrough: a new treatment called Casgevy, which leverages Crispr technology, recognized with a Nobel Prize for its gene-editing capabilities. After a long wait, he received Casgevy on December 5, marking him as one of the initial patients in the U.S. to try this innovative treatment, which was recently approved for both sickle cell disease and beta thalassemia.
Challenges in Rollout
However, the rollout of Casgevy has been slower than anticipated. Complicated manufacturing processes, insurance hurdles, and extensive preparation requirements have limited the number of patients who have received the treatment since its launch. The situation highlights the challenges of bringing revolutionary medical developments to the broader public. In parallel, another gene therapy for sickle cell, Lyfgenia, has also gained approval, but it utilizes a different method of treatment.
Accessibility Concerns
As of the latest reports, both Vertex Pharmaceuticals and Crispr Therapeutics have been reticent about providing specific figures on the number of patients treated with Casgevy. Out of 34 accredited U.S. hospitals authorized to administer the drug, only City of Hope and Children's National Hospital have confirmed administration. This raises concerns about accessibility, as several other centers are not expected to begin treatment until 2025.
The Treatment Process
“The journey to access this drug differs significantly from simply taking a pill,” remarked Leo Wang, Chow’s hematologist-oncologist at City of Hope. The one-time therapy necessitates collecting and editing the patient’s own stem cells, requiring multiple hospital stays and rounds of chemotherapy, putting potential patients at a crossroads of choice and trepidation.
Community Hesitation
Amidst the excitement of this groundbreaking treatment, a significant number of potential patients express hesitance, particularly within the Black community, which has historically experienced systemic mistrust in the healthcare system. Concerns over gene manipulation and the lengthy, intensive nature of treatment can create barriers to access and willingness to proceed.
The Path to Treatment
Chow’s path toward treatment began with consultations at City of Hope, and after receiving insurance approval, stem cell collection commenced. This process, which involves mobilization medication and apheresis, is not without risks, especially for sickle cell patients. Apheresis can lead to complications such as blood clotting, necessitating blood transfusions beforehand.
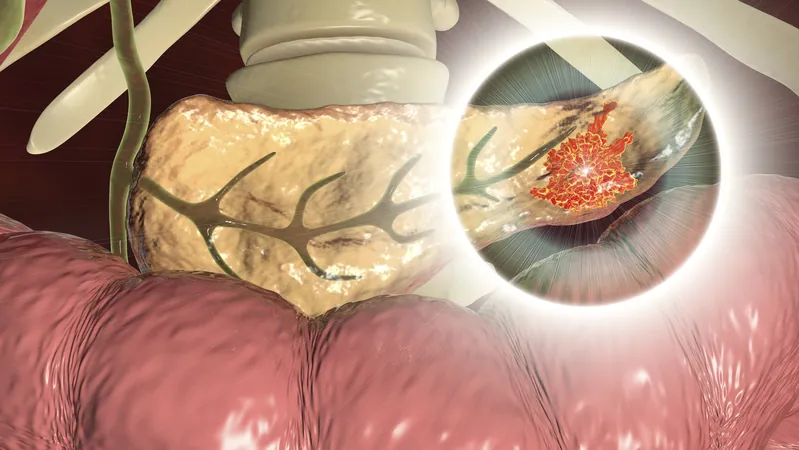
Manufacturing and Side Effects
Once the cells were successfully collected, they were sent to Vertex for editing, transforming them to produce a healthier form of hemoglobin. The entire manufacturing process can take several months, emphasizing the need for patience and trust in the medical system.
Post-Collection Challenges
Post-collection, patients can face significant challenges due to high-dose chemotherapy that creates space for the edited cells in the bone marrow. Unfortunately, this treatment comes with distressing side effects such as nausea, fatigue, and hair loss. For younger patients, there may also be long-term implications regarding fertility, as they must navigate options for preserving reproductive health.
A Hopeful Future
As Chow waits in the hospital for his body to accept the new stem cells, the community remains hopeful. Many specialists, like Edward Donnell Ivy from the Sickle Cell Disease Association of America, view this moment as the dawn of a new era in treating sickle cell disease. But navigating the reality of accessing these treatments—especially for a $2.2 million drug—continues to be an uphill battle, compounded by insurance complexities and logistical challenges faced by hospitals.
Expert Optimism and Conclusion
With demand expected to increase as awareness and success stories spread, experts like Dr. David Jacobsohn are optimistic about future developments, particularly as methods improve and potentially require less intensive chemotherapy. Ultimately, the hope remains that one day access to such therapies will be streamlined, offering a future where sickle cell disease is no longer a debilitating condition.
Chow's Vision of Hope
For Chow, the next steps are filled with mixed emotions as he clings to a vision of a pain-free future, possibly taking up hobbies like snowboarding—a prospect that once seemed impossible. While he pours his thoughts into creating rap music during his hospital stay, he also holds steadfast faith in what lies ahead, proclaiming, “It’s all in God’s hands.”

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)