The Future of Fighting Antimicrobial Resistance: Leveraging Non-Antibiotic Therapies and Cutting-Edge AI Technology
2024-09-23
Introduction
In an exciting breakthrough in the battle against antimicrobial resistance (AMR), recent research indicates that non-antibiotic therapeutic methods and artificial intelligence (AI) could be instrumental in addressing this pressing global health crisis.
The Study
The study, spearheaded by Dr. Darren Ting—a BHP Clinician Scientist Fellow at the School of Infection, Inflammation and Immunology and an Honorary Consultant Ophthalmologist at the Birmingham and Midland Eye Center—came from an international collaboration that saw contributions from esteemed institutions such as the University of Cambridge, University of Pennsylvania, University of British Columbia, and the National Laboratory of Biotechnology in Hungary, among others. The findings were published in The Lancet Microbe.
The Impact of AMR
AMR is a growing concern, with staggering figures illustrating its severity: in 2019 alone, 5 million deaths were attributed to bacterial resistance to antibiotics. The implications extend beyond fatalities; AMR leads to increased illness duration, more extended hospital stays, and soaring healthcare costs.
A Comprehensive Strategy
The team underscores that tackling AMR demands a comprehensive strategy. This includes:
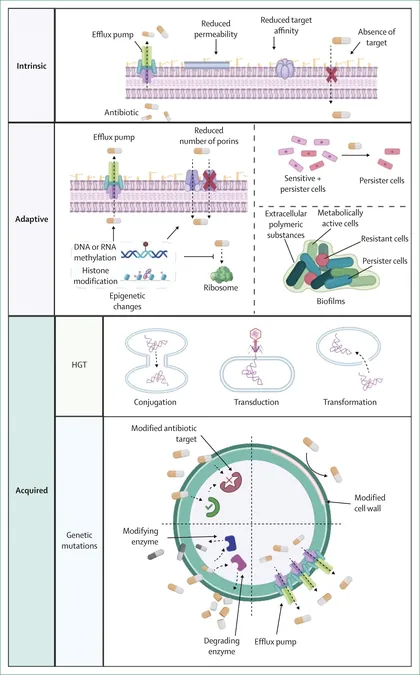
Understanding Mechanisms
Delving into the biological drivers of resistance at both individual and population levels.
Surveillance and Stewardship
Establishing robust AMR surveillance and promoting responsible antibiotic use, taking into account the choice of drugs, accurate dosages, and prescription lengths.
Enhanced Infection Control
Strengthening measures to prevent the spread of resistant infections.
Novel Therapeutic Development
Innovating new treatments such as antimicrobial peptides, bacteriophages, monoclonal antibodies, antibody-antibiotic conjugates, and gene therapies.
Harnessing AI Power
A focal point of this research is the potential of AI technologies and vast data analytics to revolutionize our approach to AMR. AI can significantly expedite antibiotic susceptibility testing—traditionally a process that spans 24 to 28 hours—by leveraging whole-genome sequencing to make faster, more accurate predictions of bacterial resistance.
Machine Learning for Surveillance
Moreover, machine learning stands to enhance large-scale AMR surveillance, particularly benefiting low- and middle-income countries where resources are often limited. AI can also refine treatment protocols by predicting the efficacy of narrow-spectrum antibiotics, thereby minimizing unnecessary second-line treatments and curbing inappropriate antibiotic prescriptions.
AI in Antibiotic Discovery
Another transformative application of AI is in the realm of antibiotic discovery. By streamlining the development process, AI has the potential to reduce the timeline for bringing new antibiotics to market from several years to mere days—a game-changer for health systems worldwide.
Conclusion
The review implores the scientific community and policymakers to foster collaborative and sustainable research efforts. Combatting AMR is not just crucial for preserving the efficacy of current antibiotics but is vital for the future of modern medicine, global health, and economic stability.
As countries grapple with the ramifications of AMR, the intersection of innovative therapeutic approaches and AI may very well hold the key to reversing this alarming trend. Will we seize this opportunity or let AMR define a new era of health challenges? The clock is ticking!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)