
The Complex Landscape of GERD: Why a Team Approach is Essential for Effective Diagnosis and Treatment
2025-01-10
Author: Siti
The Complex Landscape of GERD: Why a Team Approach is Essential for Effective Diagnosis and Treatment
Gastroesophageal reflux disease (GERD) is not just your ordinary condition; it can significantly impact one's quality of life and presents a wide array of subtypes and symptoms that make it challenging to treat. According to a recent review published in *Visceral Medicine*, addressing GERD requires a personalized, multidisciplinary strategy, especially for its more subtle forms like nonerosive reflux disease (NERD), reflux hypersensitivity (RH), and functional heartburn (FH).
The prevalence of GERD varies remarkably across different regions, ranging from 2.5% to a staggering 33%. This condition is far from uniform; it displays classic symptoms like heartburn, as well as atypical signals such as asthma and chronic coughing. Alarmingly, there has been a notable rise in younger patients with GERD, particularly within the 30 to 39 age bracket, indicating a shift in the demographic affected by this common ailment.
Understanding the Subtypes: NERD, RH, and FH
NERD is particularly intriguing because it represents GERD cases where the esophagus remains intact, despite reflux episodes. Health professionals often consider NERD as a less severe form of GERD, but this misconception may lead to untreated patients developing more severe erosive forms of the disease over time. It's critical to recognize that untreated NERD can adversely affect overall digestive health.
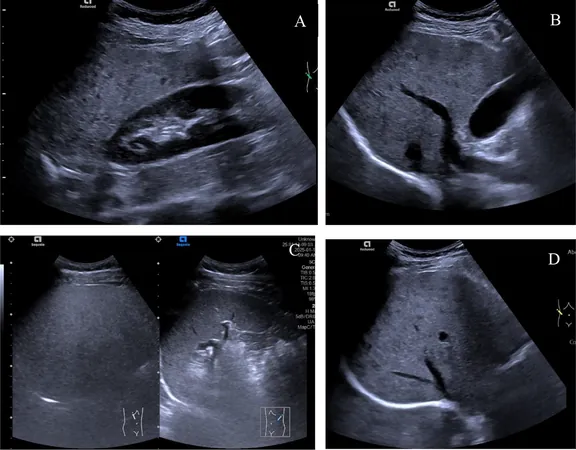
Diagnosing NERD can be a complex undertaking due to its varied clinical presentations. Tools such as 24-hour impedance-pH testing and rigorous adherence to the Lyon Consensus 2.0 criteria are essential for accurate diagnosis. Interestingly, patients with true NERD often exhibit a less pronounced response to proton pump inhibitors (PPIs) compared to those with erosive esophagitis, signaling a need for alternative therapeutic strategies.
Reflux hypersensitivity (RH) adds another layer of complexity. Patients experience chronic heartburn or chest pain without any evident structural issues, which can be disheartening and confusing. Following the Rome IV criteria for diagnosis and utilizing tools such as endoscopy and pH-impedance monitoring can help clarify the situation. Treatment methods, including PPIs and neuromodulators, show mixed efficacy and highlight the necessity for individualized care plans.
Functional heartburn (FH) presents with chronic heartburn but without typical reflux abnormalities. The management of FH is peculiar, as it often requires an approach focused on reducing esophageal hypersensitivity rather than relying solely on anti-reflux therapies, which can sometimes do more harm than good.
The Overlap with Functional Disorders and the Need for a Multidisciplinary Approach
Compounding the challenges in diagnosing GERD is the frequent overlap with other functional gastrointestinal disorders such as irritable bowel syndrome (IBS) and functional dyspepsia. This overlap can lead to a spectrum of symptoms that can complicate diagnosis and hinder effective treatment. Patients suffering from both GERD and IBS report more pronounced symptom severity and a noticeably diminished quality of life.
The review authors stress that the intricate nature of these conditions and their overlapping symptoms necessitate a team approach involving gastroenterologists, psychologists, nutritionists, and other specialists. This collaborative strategy is crucial to enhance patient outcomes and improve their overall well-being.
As ongoing research continues to unravel the complex nature of GERD and its many subtypes, it is clear that a one-size-fits-all treatment model is outdated. A tailored, multidisciplinary framework is essential for tackling the nuances of GERD effectively, ultimately leading to better management strategies and improved quality of life for patients.
In conclusion, understanding GERD's complexity and the diverse symptoms associated with its subtypes reinforces the urgent need for innovative treatments and collaborative care. As awareness and knowledge grow, so does the promise of more effective management and the hope for a better future for those battling GERD.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)