The Alarming Link Between Delay in Hip Fracture Treatment and the Risk of Deep Vein Thrombosis: What You Need to Know!
2025-04-05
Author: Siti
Introduction
A recent study sheds light on a crucial aspect of hip fracture management: the relationship between the time from injury to hospital admission (TFITA) and the likelihood of patients developing deep vein thrombosis (DVT) upon arrival. This research not only emphasizes a neglected area in trauma care but also serves as a wake-up call for healthcare systems to optimize their responses to hip fracture incidents.
Objective of the Study
The primary goal of this study was to investigate how prolonged TFITA influences the presence of DVT in patients admitted for hip fractures. Understanding this association is pivotal for developing effective prevention strategies for DVT, which can have dire consequences, including chronic pain and life-threatening complications.
Study Parameters
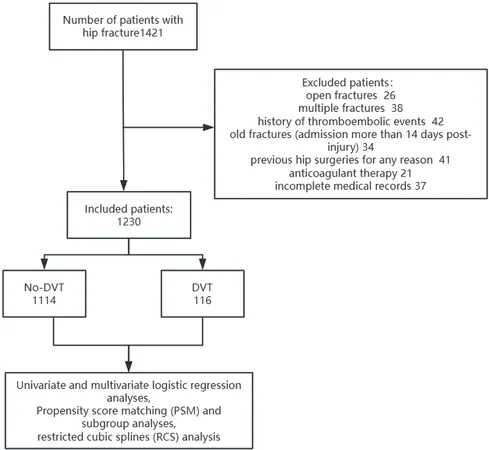
A cohort of 1,230 patients admitted with hip fractures to Chongqing Emergency Medical Center between January 2017 and December 2023 was analyzed. Various methodologies, including logistic regression and propensity score matching (PSM), were employed to assess the impact of TFITA on DVT. Moreover, researchers examined potential confounding factors such as age, injury type, and laboratory findings to provide a comprehensive overview of the risks involved.
Key Findings
The data revealed a concerning trend: patients with longer TFITA exhibited a significantly higher incidence of DVT at admission. Out of 1,230 patients studied, 116 were found to have DVT. Alarmingly, the analysis showed that for every additional hour of delay in admission post-injury, the likelihood of developing DVT increased notably. Specifically, those with a TFITA of 36 hours or more faced nearly double the risk of DVT compared to those admitted sooner.
Further investigations highlighted that older age, low-energy injuries, elevated D-dimer levels, and low platelet counts were significant risk factors associated with DVT occurrence. These findings underscore the importance of timely medical intervention.
The Implications of Delayed Admission
The relationship between delayed admission and the development of DVT can be attributed to several intertwined factors. Immobilization post-fracture can lead to decreased venous blood flow, which, coupled with systemic inflammation due to the injury, creates an environment conducive to clot formation. The healing process following a hip fracture also exacerbates the risk of vascular complications, increasing the urgency for prompt treatment.
The ramifications of DVT are severe. Without timely intervention, patients risk developing life-threatening pulmonary embolism (PE), which can result in death within hours of trauma. Therefore, understanding and addressing the factors contributing to extended TFITA is crucial for preventing DVT and improving patient outcomes.
Recommendations for Prevention
Given the findings, healthcare providers should prioritize reducing TFITA to mitigate the risk of DVT. Implementing strategies such as rapid transfer protocols, better education for caregivers, and streamlined admission processes can significantly impact patient care.
Patients presenting with hip fractures should be assessed urgently using tools like the Wells score for DVT risk stratification. Early introduction of anticoagulant therapy and the use of mechanical prevention devices, such as compression stockings, can contribute to managing risk effectively.
Conclusion
This study highlights a vital area in hip fracture care that has been largely overlooked: the impact of admission delays on DVT risk. With a clear link established, it’s imperative that healthcare systems take decisive measures to ensure timely treatment. Not only can this save lives, but it can also enhance the overall recovery trajectory of hip fracture patients. The clock is ticking—let’s make every moment count!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)