The Alarming Connection Between Monkeypox and Type 1 Diabetes: What You Need to Know
2025-06-14
Author: Jia
Unveiling Monkeypox: A Brief History
Monkeypox virus (MPXV) first graced our world in 1958, when it was spotted among laboratory monkeys by virologist Preben C. A Magnus. Though it was first identified in the Democratic Republic of Congo in 1970, evidence suggests this virus has been lurking around since at least 1899, with startling findings even linking it to Egyptian mummies!
The Zoonotic Threat: How Monkeypox Spreads
This enigmatic disease is endemic in Africa, primarily spreading through contact with infected animals like rodents and monkeys—ironically, not just monkeys, as the name implies. Human transmission can occur through direct contact with an infected individual, and alarming evidence points to airborne transmission and even sexual transmission as potential vectors.
Incubation and Symptoms: What to Expect
Once contracted, symptoms kick in after an incubation period of 10-14 days, followed by fever, headaches, and a rash that typically erupts on day three. While mild cases can be manageable, severe strains can see mortality rates spiking between 10-17%, with complications such as bronchopneumonia and encephalitis lurking dangerously close.
Recent Outbreaks: A Growing Concern
While the first major outbreak outside Africa occurred in the U.S. in 2003 via infected prairie dogs, the 2022 WHO alert signals a worrying escalation, particularly in non-endemic countries like Canada and Spain. By May 2024, cases skyrocketed—with a concerning number of infections in children and a 5.3% fatality rate.
Monkeypox and Type 1 Diabetes: The Unraveling Link
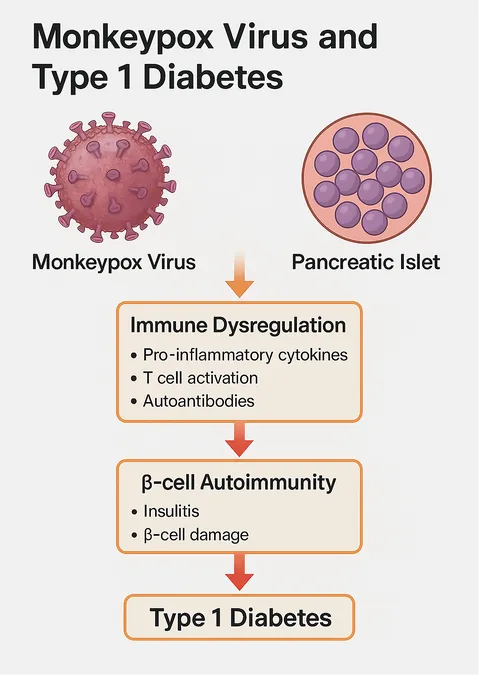
Emerging research points to a disturbing potential link between MPXV and Type 1 Diabetes (T1D), an autoimmune disorder that wreaks havoc on pancreatic beta cells, resulting in high blood sugar levels. Often triggered by viral infections, there’s growing evidence that MPXV may play a role in exacerbating T1D, albeit the mechanics are not yet fully understood.
The Autoimmune Dilemma
T1D is primarily characterized by an autoimmune attack on insulin-producing cells in the pancreas. Notably, recent studies have reported pancreatic damage in patients with severe MPXV infections, raising eyebrows at the possibility of a connection. Could MPXV be adding fuel to the fire of autoimmune responses?
Inflammatory Signaling: The Biological Backdrop
MPXV infection sets off a complex inflammatory cascade that may trigger or worsen autoimmune diseases like T1D. The virus releases pro-inflammatory cytokines that can interfere with immune function, highlighting the dire need for further research into its role in immune-related disorders.
The Call for Action: Implications for Public Health
Given these emerging insights, it’s imperative to take a closer look at MPXV’s potential role in triggering T1D. Public health strategies and treatments targeting inflammation could not only mitigate the impact of monkeypox but may also lower the risk of diabetes, especially in vulnerable populations.
Final Thoughts: Navigating the Future of Health
The links between MPXV and diabetes are still being unraveled, but the implications are clear: we must remain vigilant. As outbreaks continue, understanding these connections is essential for public health responses and for safeguarding vulnerable populations from diseases that threaten to add further strain on healthcare systems.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)