Tailored COVID-19 Vaccination Strategies: A Must for Lupus Patients, New Study Reveals!
2025-01-15
Author: Jia
Groundbreaking Study Unveiled
A groundbreaking study conducted by researchers at Emory University has uncovered alarming insights into the effectiveness of mRNA COVID-19 vaccines for patients with autoimmune diseases, particularly lupus. Published in *Nature Immunology*, this research reveals that lupus patients may require customized vaccination strategies to improve their protection against COVID-19.
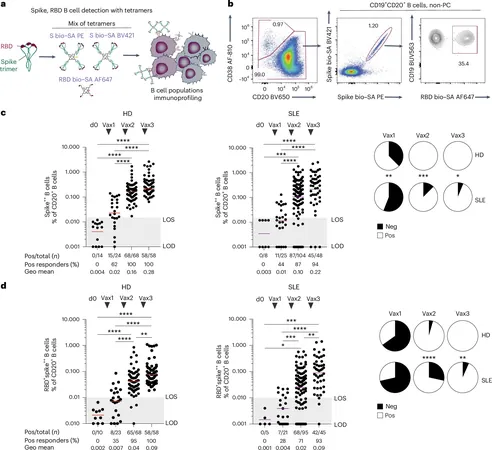
For the first time, this study demonstrates that vaccine-induced immune responses produce a novel type of memory B cell, which could play a critical role in bolstering booster responses and protection against infections. However, the long-term immunity these newly discovered cells provide, especially against future infections, is still under investigation.
What is Lupus?
Systemic Lupus Erythematosus (SLE), commonly known as lupus, is a chronic autoimmune disease where the immune system mistakenly attacks healthy tissues, leading to widespread inflammation and a variety of symptoms, including fatigue and joint pain. With the onset of the COVID-19 pandemic in 2021, understanding the efficacy of vaccines in vulnerable populations, such as those with lupus, became paramount.
Katia Faliti, Ph.D., the lead author of the study and an instructor at Emory University's Department of Medicine, expressed the significance of these findings. "This research sheds light on how vaccine-induced immune responses develop and persist in individuals with autoimmune conditions like lupus," she explained.
Study Details
The study was comprehensive, involving 79 lupus patients and 64 healthy controls. Researchers focused on the role of B cells—white blood cells integral to the immune response. While mRNA COVID-19 vaccines successfully generated neutralizing antibodies and immune memory in healthy individuals, the results were strikingly different for lupus patients. The study revealed that 10% to 30% of lupus patients produced B cells that did not target the vital spike protein of the COVID-19 virus at all.
Researchers identified a concerning trend: a specific subset of B cells, termed DN2 B cells, was found in considerably higher frequencies in lupus patients post-vaccination. This increased presence correlated with a diminished neutralizing antibody response, significantly impacting the vaccines' protective efficacy.
Dr. Iñaki Sanz, a professor of immunology at Emory and senior author of the study, added, "Our previous work established a link between DN2 B cells and the severity of lupus, particularly among women of Black ancestry. Now we see that the activation of these cells in response to the vaccine is not only persistent but might overwhelm the immune response in lupus patients."
The Implications for Future Vaccination Strategies
The findings from this study suggest that a one-size-fits-all vaccination approach may not be effective for every patient, particularly those with autoimmune diseases. As the consequences of lingering effects from both the disease and the vaccine are further examined, there is growing hope for the development of tailored vaccination strategies that could significantly enhance immunity for lupus patients and others with similar conditions.
As researchers continue to explore these important insights, the overall goal remains clear: to ensure that vulnerable populations receive the protection they need against COVID-19. This groundbreaking research not only offers hope for lupus patients but could also pave the way for personalized medicine strategies in autoimmune disorders more broadly.
Conclusion
Stay tuned as we follow this evolving story—it's a crucial development that could change how we approach vaccinations for some of our most vulnerable communities!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)