Surprising Link Between Mucin Sialylation and Mucus Transport in Lung Health
2024-09-24
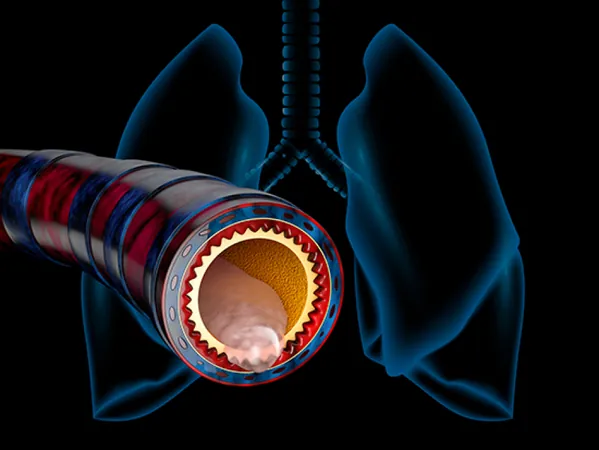
Breathing is an essential part of our existence, but with every inhale, our lungs can also take in harmful microbes. Fortunately, mucus plays a crucial role as a protective barrier within the airways. This gel-like substance traps bacteria, viruses, dust, and pollen, working tirelessly to safeguard our lungs. Tiny, hair-like structures known as cilia then help move this mucus up and out of the airways.
But what happens when the body produces excess mucus that is thick and dry? This thickened mucus can obstruct airways and overwhelm the lungs’ natural clearance mechanisms, creating an ideal environment for entrapped microbes to thrive. Such complications can lead to serious muco-obstructive diseases, including cystic fibrosis (CF).
A groundbreaking study conducted by researchers at the University of Alabama at Birmingham (UAB) reveals a critical connection between mucus composition and lung health. Led by Dr. Jarrod W. Barnes and Dr. Steven M. Rowe, the team explored how a sugar modification affects mucin, the primary component of mucus. Their findings, published in Scientific Reports, highlight the importance of a sugar called sialic acid in the formation and transport of mucus.
Mucus is made up of mostly water and mucins—large protein molecules adorned with sugars. The research indicated that when sialic acid levels in MUC5B, a major airway mucin, are reduced, the mucus becomes more compact and less able to move. This reduction leads to an alarming transformation into a low-charged form of the mucin, which has been previously linked to conditions like cystic fibrosis and asthma.
Through various analytical methods, including transmission electron microscopy, the researchers illustrated that decreased sialylation results in tangled MUC5B polymers. This entangled state negatively impacts mucus transport in human bronchial cells and rat airway models, suggesting that mucin charge plays a pivotal role in the pathology of muco-obstructive diseases.
Interestingly, the study also discovered that CF patients exhibit lower levels of an enzyme known as ST3Gal1, which is responsible for adding sialic acid to mucin proteins. However, treatment with specific drugs—Elexacaftor, Tezacaftor, and Ivacaftor, known as correctors for the cystic fibrosis transmembrane conductance regulator (CFTR)—partially restored the function of this enzyme.
This research offers a potential therapeutic pathway for treating cystic fibrosis and other debilitating muco-obstructive diseases, including chronic obstructive pulmonary disease (COPD), primary ciliary dyskinesia, and non-cystic fibrosis bronchiectasis.
The findings underscore the need for further investigation into mucin sialylation as a target for therapeutic intervention. The implications for improving lung health and combating chronic respiratory diseases are enormous, setting the stage for future advancements in treatment strategies.
Stay tuned as science uncovers more secrets about the critical role of mucus in our respiratory system and how we can harness that knowledge to fight diseases!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)