Single Antiplatelet Therapy Outshines Dual After TAVI: Shocking TRITAVI Findings!
2024-11-05
Author: Daniel
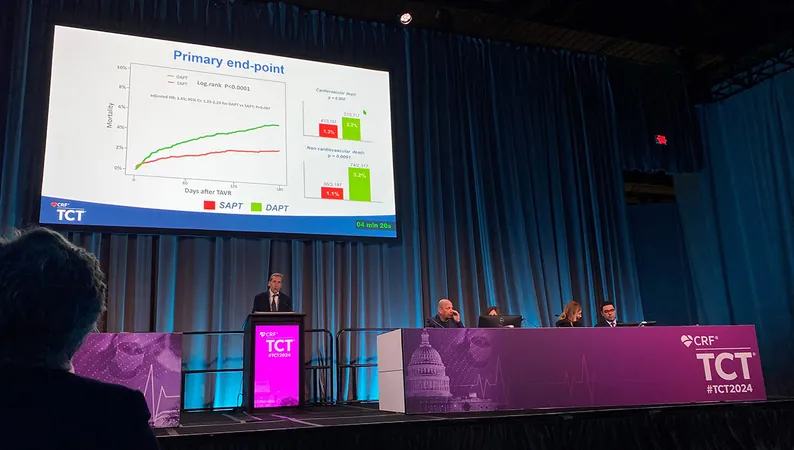
In a groundbreaking revelation from the TRITAVI registry presented at TCT 2024 in Washington, DC, researchers have unveiled that patients undergoing Transcatheter Aortic Valve Implantation (TAVI) may benefit more from a single antiplatelet therapy (SAPT) compared to the traditional dual antiplatelet therapy (DAPT). This astonishing finding highlights a lower risk of all-cause mortality and major bleeding after just six months on SAPT.
The results from the TRITAVI study align with previous research, including the POPular TAVI trial, which also emphasized that most TAVI patients respond favorably to single antiplatelet therapy. However, it is essential to note that patients with a heightened risk of ischemic events or those with established coronary artery disease (CAD) might still require DAPT.
Consistent with the European guidelines published in 2021, which recommend lifelong single antiplatelet therapy with aspirin or clopidogrel for TAVI patients without an existing need for oral anticoagulation, the evidence is compelling. The 2020 US guidelines also advocate for single therapy, though with less intensity.
Dr. Francesco Pelliccia from Sapienza University of Rome, who led the presentation of the TRITAVI results, pointed out the alarming variability in antithrombotic protocols across the 20 participating centers. This disparity underscores the urgent need for standardized treatment guidelines to ensure optimal patient care.
Key Findings from the TRITAVI Study:
The study monitored 5,514 TAVI patients across 20 European centers from 2012 to 2022. Patients with prior anticoagulation, nonfemoral TAVI, procedural complications, or a recent history of acute coronary syndrome or percutaneous coronary intervention were excluded.
In the study, 3,197 patients were treated with single antiplatelet therapy (average age 81.3 years; 50.8% male), while 2,317 received dual therapy (average age 81.8 years; 45.2% male). The DAPT group exhibited a higher prevalence of risk factors like hypertension and previous myocardial infarction.
Notably, single antiplatelet therapy resulted in a one-third reduction in all-cause mortality compared to DAPT at six months. Major bleeding occurrences were also significantly lower (0.5% vs. 1.3% for SAPT versus DAPT).
Interestingly, the study revealed that a history of DAPT use emerged as a predictor for all-cause mortality (adjusted HR 1.65; 95% CI 1.22-2.23), alongside other risk factors.
Despite these promising results, questions remain about optimal antiplatelet strategies. Experts, including Dr. Victor Alfonso Jimenez Diaz, are exploring whether more potent P2Y12 inhibitors might offer better protection against ischemic events while reducing bleeding risks. The potential issue of subclinical leaflet thrombosis also raises concerns that have yet to be addressed.
The TRITAVI registry findings are set to reshape clinical practice and reinforce the importance of personalized treatment approaches in TAVI patients. As the medical community digs deeper into these revelations, the emphasis on utilizing single antiplatelet therapy may pave the way for improved patient outcomes in the future.
Stay tuned as we continue to follow this evolving story that could change the landscape of cardiology!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)