
Shocking Study Reveals How Pharmacy Closures Endanger Lives of Patients on Anticonvulsants!
2024-11-04
Author: Sarah
Introduction
In a groundbreaking new study published in the Journal of the American Medical Association, researchers have revealed a startling connection between pharmacy closures and the refill rates of anticonvulsant medications, essential for managing epilepsy, neuropathic pain, and psychiatric disorders. Alarmingly, missed doses of these critical medications can lead to increased mortality, heightened pain, and a surge in emergency room visits, endangering countless lives across communities in Colorado.
Research Details
The research team, spearheaded by Dr. Kelly Anderson, an assistant professor at the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, aimed to assess how closures of local pharmacies affect access to a Medicare-protected class of medications that must be covered by Medicare prescription drug plans.
Study Findings
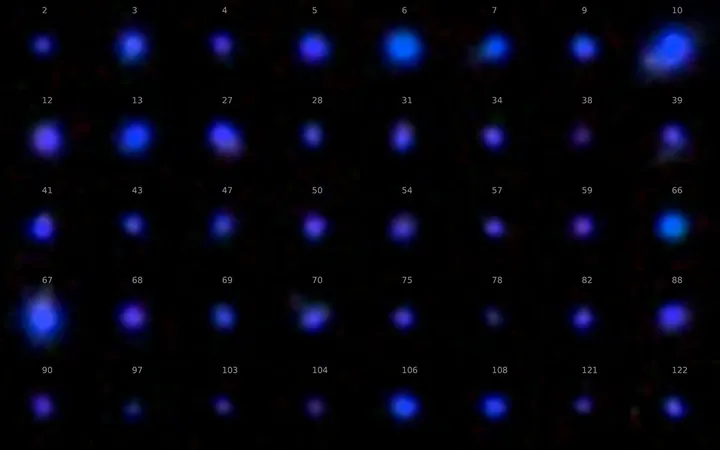
Using comprehensive all-payer claims data from Colorado, the study identified 39 pharmacy closures between January 2018 and June 2022. The findings were striking: there was a 15.6% decrease in anticonvulsant medication refills and a staggering 14.4% reduction in the total days' supply patients received post-closure. What's more, the negative impact on medication refills persisted for up to six months following a pharmacy's closure, highlighting a prolonged crisis for patients who depend on these vital treatments.
Expert Insights
Dr. Anderson noted, 'While some patients have turned to mail-order pharmacies as a workaround, our findings show that these services are not sufficient to fill the gap left by local pharmacy closures.' This revelation emphasizes the urgency of the situation and raises questions about the accessibility of medications for vulnerable populations.
Wider Implications
This study adds to a growing body of evidence indicating that pharmacy closures also adversely affect the refill rates of cardiovascular medications. Dr. Anderson emphasized the need for the U.S. healthcare system to proactively address these issues, suggesting strategies such as providing 90-day medication supplies before anticipated closures, offering financial support to pharmacies in underserved regions, and encouraging healthcare providers to assist patients in transferring prescriptions efficiently.
Conclusion
As we continue to uncover the ramifications of pharmacy closures, it becomes increasingly clear that systemic changes are essential to protect patient health and ensure uninterrupted access to life-saving medications. The implications of these findings are profound, highlighting an urgent need for actionable solutions to support those at greatest risk.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)