Shocking Link Discovered: How Gestational Diabetes Can Propel Women to Type 2 Diabetes – New Biomarker Research Unveiled!
2025-01-14
Author: Siti
A groundbreaking new study reveals that 35% of women who experience gestational diabetes are likely to develop type 2 diabetes within ten years following childbirth. Spearheaded by Dr. Saifur Khan, a robust cardiology research faculty member at the University of Pittsburgh Vascular Medicine Institute, this research marks a pivotal point in understanding the molecular mechanisms that trigger this progression.
In this eye-opening study published in Science Advances, Dr. Khan emphasizes the urgent need for innovative detection and preventative strategies. “Many women with a history of gestational diabetes are developing type 2 diabetes at remarkably young ages, often before they even turn 40,” he states. This alarming trend calls for urgent action to identify root causes and develop targeted therapeutic interventions.
The research team particularly focused on a group of 143 Hispanic women aged between 20 and 45, all of whom had previously battled gestational diabetes. Disturbingly, out of these, 65 women transitioned to type 2 diabetes within a mere eight years post-delivery. The remaining 78 women served as control subjects to highlight the stark differences in biomarker levels.
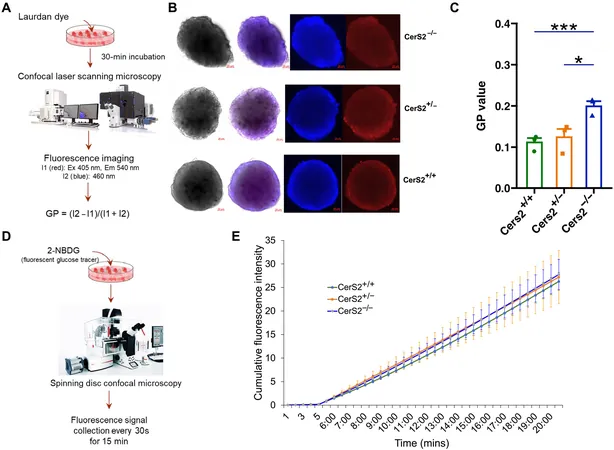
By meticulously analyzing human metabolomic, lipidomic, and genomic data, the researchers discovered that women who later developed type 2 diabetes exhibited significantly lower levels of sphingolipids—specific lipids crucial for cellular function—compared to their counterparts. This diminished production of sphingolipids was linked to a mutation in a gene named CERS2, underscoring its potential role in the progression toward type 2 diabetes.
Drawing from their findings, it became clear that the decreased presence of these lipid molecules could serve as an early warning signal for women at risk of transitioning from gestational diabetes to a chronic type 2 condition. “The implications of these insights are substantial,” notes Dr. Khan, also affiliated with the VA Medical Center in Pittsburgh. “This could lead to innovative therapeutic strategies that focus on the sphingolipid metabolic pathway.”
Future research is set to delve deeper into how the loss of CERS2 function affects pancreatic health and contributes to abnormalities in insulin secretion and glucose regulation. Experts believe that restoring normal sphingolipid metabolism by either enhancing CERS2 activity or countering its negative effects on pancreatic functions could bring about a much-needed improvement for high-risk individuals.
Collaborators on this significant study include distinguished researchers from various institutions, ensuring a wide-ranging expertise that fortifies the findings of this alarming progression from gestational to type 2 diabetes.
With this new knowledge at our fingertips, could we be on the brink of a revolutionary approach to combat diabetes in women? Stay tuned as the implications of this research unfold, inspiring hope for early detection and prevention strategies that could change lives.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)