Shocking Insights on Malaria and Hepatitis Infections Revealed in North Central Nigeria!
2024-11-16
Author: Yu
What They Found: A Closer Look at Inclusion and Exclusion Criteria
The study included a diverse group of 248 participants, ranging from young children to individuals over 81 years old. Patients presenting symptoms suggestive of malaria, hepatitis B Surface Antigen (HBsAg), or Hepatitis C Virus (HCV) were closely examined. Notably, individuals recently treated for these infections were excluded to ensure the accuracy of prevalence estimates. It aimed to consider various factors such as socioeconomic status, occupation, and healthcare access to capture a true reflection of disease prevalence among different demographics.
The Data Collection Process
Data was meticulously gathered using a reliable semi-structured questionnaire and blood samples were analyzed for malaria, HBsAg, and HCV using advanced testing methods. The results yielded a revealing picture of the infection landscape within the community, presenting a 52.4% malaria prevalence rate among participants. This stark figure highlights the pressing health crisis posed by malaria in the region—a concern shared by many neighboring countries as well.
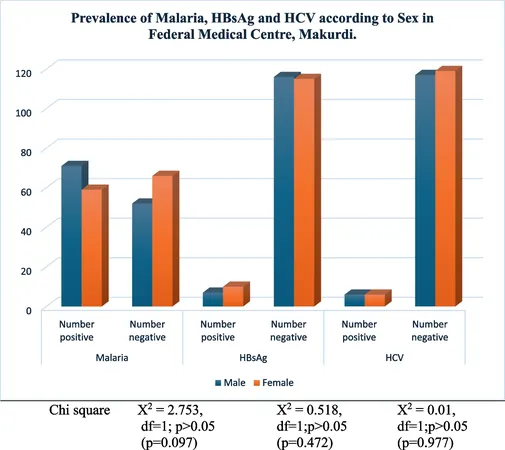
Gender and Age Dynamics
Gender differences were evident in malaria prevalence, with 57.7% of males testing positive compared to 47.2% of females, although the difference wasn't statistically significant. Age-wise, individuals aged 26-40 years were the most affected, drawing attention to the need for targeted intervention strategies aiming at this vulnerable demographic.
Marital Status Doesn't Matter?
Interestingly, the study reported no significant differences in malaria prevalence based on marital status, suggesting that both singles and married individuals faced similar risks. The prevalence for HBsAg stood at 6.9%, showing no considerable statistical significance between married and single patients.
The Role of Income Levels in Disease Prevalence
Income emerged as a noteworthy factor; individuals categorized as low-income showed a malaria prevalence of 52.6%, while no cases arose in the high-income group. However, hepatitis infections revealed a contrasting story—those in the middle-income bracket had higher HCV positivity rates. This emphasizes how socioeconomics can shape health outcomes in complex ways, required for public health strategists to consider.
Clinical Manifestations and Testing Results
Patients' clinical symptoms were predominantly associated with malaria, particularly fever, reported in 57.7% of malaria-positive individuals. Despite this, specifics symptoms didn’t strongly correlate with the likelihood of malaria infection—highlighting the need for rigorous testing irrespective of symptom presence. Use of insecticide-treated nets (ITNs) proved beneficial with a significant reduction in malaria cases among users compared to non-users (46.8% vs. 70.7%), thus underscoring their vital role in malaria control.
Wider Implications and Call to Action
The findings of this study signal alarm bells for health authorities in Nigeria, as public health strategies must evolve to tackle the distinct challenges posed by socioeconomic disparities. Continuous screening, education about preventive measures, and improving access to healthcare are imperative.
Future Directions: More Research Needed
Moving forward, researchers suggested areas for further exploration, including the effectiveness of specific interventions targeting at-risk groups, enhancing blood screening methods, and understanding the long-term effects of chronic infections. With the stakes this high, will this study compel the Nigerian government to ramp up its efforts in combating these pervasive health threats? The public is left wondering how quickly these startling insights will translate into impactful policies to safeguard communal health.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)