Shocking Findings on the Safety of PEG Tubes in HIV Patients Revealed
2024-12-31
Author: Arjun
Background
Percutaneous Endoscopic Gastrostomy (PEG) tube insertion is increasingly recognized as a lifeline for patients unable to consume nutrition orally. This critical procedure, often required for long-term nutritional support in various populations—including those with neurological disorders, advanced malignancies, and HIV—does not come without risks. PEG placements can lead to complications such as bleeding and infections, yet the specific outcomes and risks associated with HIV patients remain inadequately explored. The urgency to understand the implications of PEG tubes for HIV-positive individuals is highlighted by their increasing prevalence in clinical settings.
Methods
In an extensive study involving 639 PEG placements among 461 unique patients, 85 of whom were HIV positive, researchers meticulously analyzed complication rates and mortality outcomes. This investigation, carried out at Bronx Care Health System, meticulously monitored these patients over time. The aim was to juxtapose the experiences of those living with HIV against their HIV-negative counterparts in relation to post-PEG outcomes.
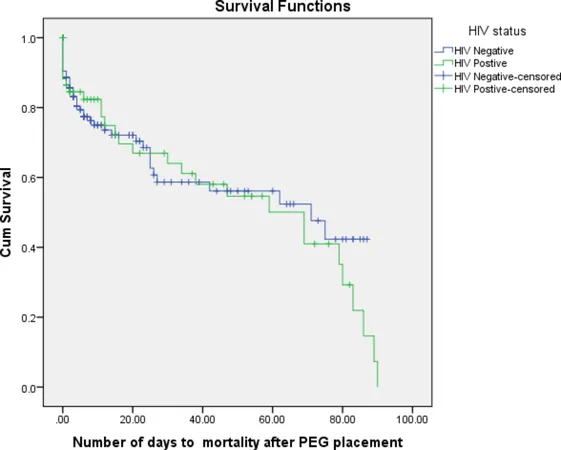
Results
The results were startling. After PEG insertion, post-procedure bleeding was significantly higher in HIV patients (15.3%) compared to 4.5% in non-HIV patients (p < 0.001). Alarmingly, the study found a stark contrast in 1-year mortality rates—37.6% for HIV patients versus 17.8% for those without HIV (p < 0.001). This prognosis raises critical questions about patient management and choices surrounding PEG procedures in vulnerable populations.
Conclusion
These findings force us to reevaluate clinical guidelines and patient care strategies for PEG procedures involving HIV-positive individuals. There’s an evident need for heightened awareness and specialized management, taking into account the increased risks of bleeding and higher mortality rates observed in this demographic. Future research is crucial to uncover the biological and treatment-related factors leading to such worrying outcomes.
Study Design and Context
This retrospective observational study spanned from 2004 to 2016, garnering Institutional Review Board (IRB) approval and adhering to ethical guidelines. The patient selection was stringent, ensuring only those admitted during this timeframe who underwent the PEG procedure were included, paving the way for a robust analysis of various demographic factors and laboratory results.
HIV Status and Risk Mechanics
Uniquely, HIV status was established through clinical documentation and testing, with a clear focus on how this status correlated to post-operative results. What sets this study apart is the nuanced understanding of coagulopathy in HIV patients due to the nature of the virus and antiretroviral treatments, which complicate their physiological responses during and after medical procedures.
Comparative Analysis and Training Insights
Surprisingly, there appeared to be comparable baseline lab parameters between the two groups, with exceptions like slightly elevated INR levels in HIV patients. More striking, though, was the noteworthy revelation that advanced age and existing comorbidities, often silent predictors of patient outcomes, did not significantly differ between HIV and non-HIV patients in this population—suggesting a potentially unique pathophysiological challenge among those with HIV.
Calls for Action
The pressing call for further exploration into the raised mortality rates amongst HIV patients post-PEG indicates an urgent need for systematic approaches to care that are deeply informed by these findings. By prioritizing targeted interventions and meticulous monitoring, clinicians can better navigate the complexities of care for HIV-positive individuals requiring PEG placement.
Final Thoughts
This study not only contributes to a growing repository of knowledge about PEG outcomes in specific patient populations but emphasizes the necessity for routine scrutiny of clinical procedures among high-risk patients. In light of these shocking findings, medical professionals must advocate for improved protocols and explore tailored treatment paths for those standing at the intersection of HIV and nutritional rehabilitation. The stakes are high; lives depend on it.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)