Shocking Findings: COVID-Positive Nursing Home Staff Could Be Hurting Patients More Than Helping!
2024-09-25
A groundbreaking study recently published in JAMA Network Open reveals a troubling connection between sending mildly ill nursing home staff home due to COVID-19 and worsened health outcomes for residents. The research highlights that this practice not only exacerbates understaffing but also leads to increased hospitalizations, deaths, and financial burdens for nursing homes.
With the current landscape of nursing home staffing, a staggering 94% of facilities were reported to be understaffed in 2021. Fast forward to 2024, and 72% of nursing homes still have fewer staff than before the pandemic began. Factors such as low wages, challenging working conditions, high turnover rates, and a lack of mandated minimum staffing levels contribute to this ongoing crisis.
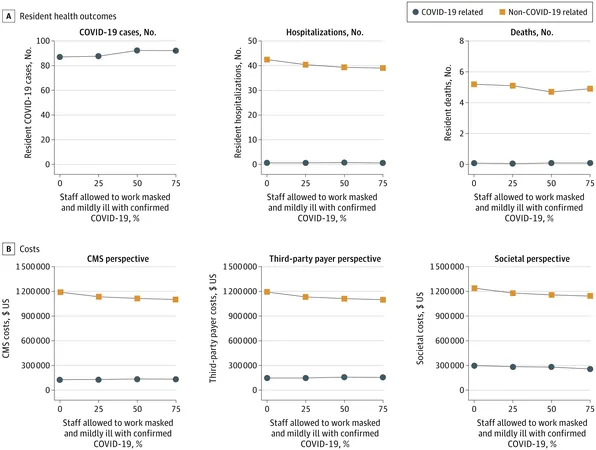
The study's findings indicate that 22% of resident care tasks go uncompleted simply due to current staffing inadequacies. Annually, this could mean as much as 34,185 missed care tasks per nursing facility, resulting in approximately 38 hospitalizations and 4.6 deaths per 100 beds, translating into over $1 million in costs for the Centers for Medicare and Medicaid Services (CMS).
As the pandemic unfolded, health authorities recommended sending COVID-positive staff home to minimize the spread of the virus. However, this decision has inadvertently led to 649.5 more missed tasks each year, equating to 1.8 additional tasks left unfinished daily. The result? An alarming rise in hospital admissions and fatalities resulting from insufficient care, costing an extra $247,090 per year.
In a surprising twist, the study proposes an alternative solution: allowing mildly ill staff to continue working with N95 respirators. This strategy could drastically reduce missed workdays—by an average of 240 days annually—and improve task completion, resulting in 3.5 fewer hospitalizations and 0.4 fewer deaths. While allowing mildly ill staff to work increased the number of resident COVID-19 cases slightly, it maintained similar hospitalization rates, offering a potential pathway to alleviating nursing home crises without sacrificing patient care.
The financial implications also are significant; this approach could save an average of $85,470 each year per facility.
Bruce Y. Lee, a key author of the study and a professor at CUNY SPH, cautions, 'While our research suggests allowing mildly ill staff to work reduces understaffing and minimizes harm, we must not encourage employees to work while sick and contagious.'
A call to action resonates throughout this research: the imperative to address the root causes of understaffing in nursing homes. To truly safeguard the well-being of residents, it's essential to reform wage structures and working conditions that have plagued this sector for years.
This eye-opening study serves as a stark reminder that the ripple effects of COVID-19 continue to shape healthcare practices. Are we willing to change our approach to protect our vulnerable populations? The time for urgent action is now!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)