Shocking Case of Eosinophilic Gastrointestinal Disease Causing Liver Abscess in 68-Year-Old Patient
2024-11-15
Author: Jia
In an unexpected turn of events, a 68-year-old man walked into our clinic with distressing symptoms of abdominal distension and nausea that had lingered for an entire week. Initially treated for suspected acute gastroenteritis with conventional antibiotics at a local hospital, his condition showed no signs of improvement. Remarkably, the patient reported no recent travel, had no contact with sick individuals, and had a clean history of tobacco, alcohol, or illicit drug use. His family history also showed no similar issues, making this case particularly intriguing.
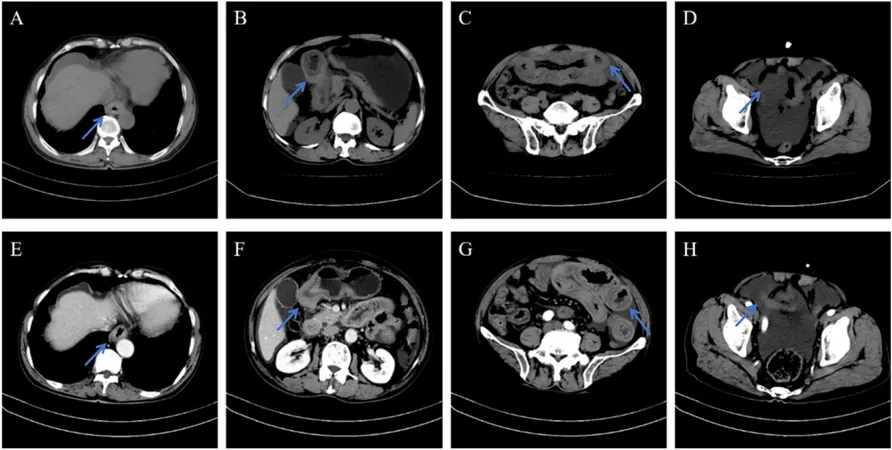
Upon examination, the man had a noticeably distended abdomen with a shifting dullness. Blood tests revealed concerning results: a white blood cell count of 13.3 x 10^9/L, elevated eosinophils at 5.56 x 10^9/L, and Total IgE at 455.3 IU/mL. To add to the intrigue, a CT scan unveiled significant edema and wall thickening in key areas of the gastrointestinal tract, as well as a troubling liver abscess.
An abdominal paracentesis allowed for a deeper investigation, highlighting an alarming 34% of eosinophils in the ascitic fluid. Not stopping there, a liver abscess puncture and drainage followed, with subsequent metagenomics next-generation sequencing (mNGS) revealing the presence of Klebsiella pneumoniae (KP)—an opportunistic pathogen. No fungal, viral, or parasitic infections were detected, leaving us with more questions than answers.
The gastroenterological examination was equally revealing. Endoscopy displayed significant edema in the esophagus and gastric antrum, while colonoscopy showed suspicious erythema throughout the colon. Biopsies from various sites confirmed our fears: substantial eosinophilic infiltration—a strong indicator of eosinophilic gastrointestinal diseases (EGIDs).
With a cacophony of tests pointing towards no malignancies or parasitic infections, a life-altering diagnosis of EGIDs complicated by a Klebsiella liver abscess was made. The urgency was palpable, and the patient was placed on a robust regimen of 2g of cefoxitin administered intravenously twice daily. Interestingly, glucocorticoid therapy was sidelined due to the risk of exacerbating the existing liver abscess.
After a diligent 10-day course of antibiotic treatment, a follow-up ultrasound showed a promising reduction in the size of the liver abscess. The patient was discharged with a prescription for cefixime and a promise of tight follow-up care. Remarkably, during a follow-up visit, lab results demonstrated a decrease in the eosinophil count from 5.56 x 10^9/L to a healthier 0.65 x 10^9/L within just two weeks!
This case underscores the puzzling complexity of EGIDs and their potential to facilitate severe complications like pyogenic liver abscesses (PLA). While Klebsiella pneumoniae often lurks as a sinister opportunist, the interplay of gut dysbiosis—often exacerbated by antibiotic treatments—becomes a crucial factor leading to translocation across the intestinal barrier and ensuing liver infections.
The implications of this case shed light on the urgent need for heightened awareness regarding gastrointestinal health and the role eosinophils play in maintaining the body's defenses. As research continues, we may uncover even more connections between these seemingly unlinked conditions, highlighting the importance of gut health for overall well-being.
Stay tuned for future insights into the evolving understanding of eosinophilic gastrointestinal diseases and their systemic effects—this story is far from over!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)