Shocking Case of Bilateral Primary Vitreoretinal Lymphoma Misdiagnosed as Fungal Endophthalmitis!
2024-12-30
Author: Yu
Introduction
A 60-year-old male patient arrived at the clinic complaining of blurriness in both eyes over the past 15 days. Initially misdiagnosed as suffering from intermediate uveitis, he had undergone treatment with oral corticosteroids, which unfortunately led to secondary glaucoma and complicated cataracts.
Medical History
Two months prior to this incident, he had cataract surgeries in both eyes, one week apart, and was on topical steroids and anti-glaucoma medication. His medical history included diabetes, hypertension, and coronary artery disease, and he also spent time in intensive care due to a COVID-19 infection, receiving high doses of systemic steroids during his recovery.
Initial Assessments
After the cataract surgeries, he seemed to improve. However, six weeks later, his vision worsened again, accompanied by bilateral dense vitritis and yellowish sub-retinal deposits that mimicked exudates. Initial assessments pointed towards a potential case of endophthalmitis.
Diagnostic Procedures
To rule out infection, urine and blood cultures were conducted but returned negative results. The patient underwent a bilateral pars plana vitrectomy (PPV) with intravitreal administration of vancomycin, voriconazole, and moxifloxacin to curb the envisioned infection.
Findings and Confirmation of Diagnosis
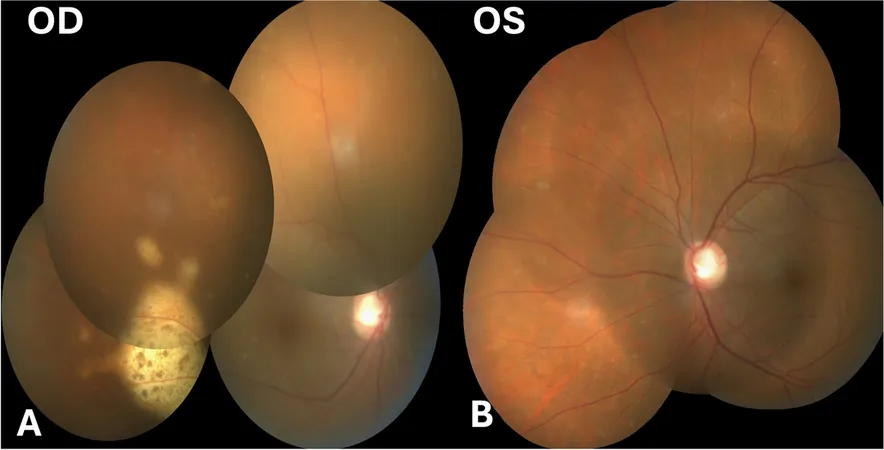
Further analysis of vitreous samples revealed no microbial growth, and a post-operative fundus examination revealed notable lesions consistent with primary vitreoretinal lymphoma (PVRL). The right eye displayed yellowish sub-retinal deposits combined with retinal pigment epithelium (RPE) changes, while the left eye showed distinct pigmented lesions.
Biopsy and Results
Imaging through spectral domain optical coherence tomography (SD-OCT) demonstrated suspicious infiltrates, leading to a decision for a sub-retinal biopsy in the right eye. During the biopsy, lymphoid cells were found in a necrotic background, confirming the diagnosis of PVRL based on cytological analysis and elevated interleukin (IL-10) levels.
Consultation and Further Imaging
Further consultation with a medical oncologist, along with fluorodeoxyglucose positron emission tomography (FDG PET) and cranial magnetic resonance imaging (MRI), revealed no systemic lymphoma, but PVRL was confirmed.
Treatment and Progress
The treatment plan involved intravitreal Methotrexate injections, which resulted in remarkable regression of the lesions. The patient transitioned to a weekly injection regimen due to epithelial toxicity in one eye, but by the 11th injection in one eye and the 8th in the other, significant clinical improvements were noted.
Follow-up and Conclusion
The latest follow-up at 18 months post-presentation showed perfect vision and normal intraocular pressure (IOP), with MRI scans indicating no central nervous system involvement. PVRL, a rare and serious condition, can often masquerade as uveitis, leading to diagnostic delays and inappropriate treatment as observed in this case.
It showcases the crucial need for healthcare providers to remain vigilant for such masquerading diseases, especially in older patients presenting with bilateral recurrent vitritis. Early diagnosis through vigilant imaging and timely biopsies can avert mismanagement and promote effective treatment, as this case compellingly illustrates.
With increasing awareness of PVRL's symptoms and prompt therapeutic interventions, we can improve outcomes and potentially save the vision of patients impacted by this aggressive ocular lymphoma. Don't miss the signs—stay informed and proactive in your ocular health!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)