Shocking Brain Discovery: How Stress Affects Your Mood and Opens New Doors for Antidepressants!
2025-04-12
Author: Daniel
Groundbreaking Research Reveals the Dual Nature of Stress on Brain Repair
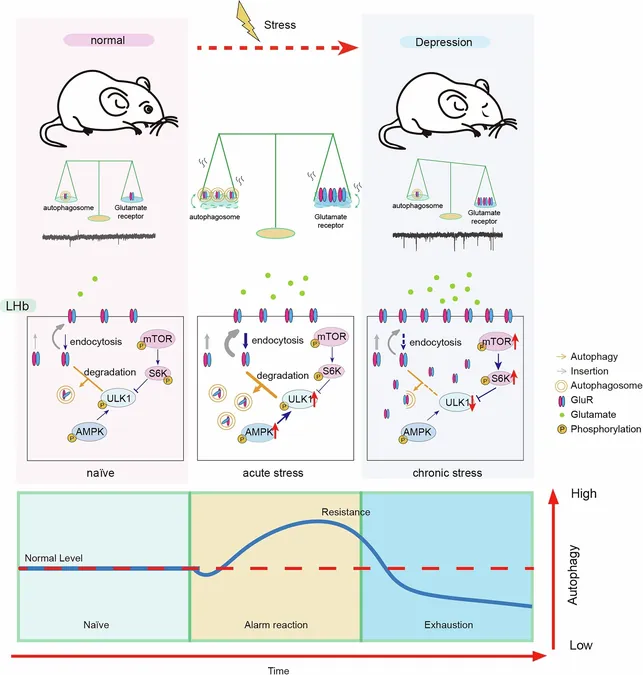
Researchers from Zhejiang University have uncovered startling differences in how acute and chronic stress affect neural repair, specifically in a brain area crucial for emotional regulation—the lateral habenula. While acute stress was found to enhance the brain's natural repair mechanisms, chronic stress dampened these processes.
Why It Matters: The Global Impact of Depression
With major depressive disorder affecting around 10.6% of the global population, understanding the role of stress in this mental health crisis is vital. Stress is not only a common part of life; it's a significant player in the onset of depression, destabilizing emotional regulation when prolonged.
The Science of Autophagy: A Key to Understanding Depression
Autophagy, the brain's cleaning mechanism for degrading and recycling internal parts, is getting increasing attention in the realm of mental health. It plays a critical role in neuronal health and has been implicated in various neurological disorders like Alzheimer's and Parkinson's disease. However, its influence in stress-related psychiatric issues was not fully understood—until now.
The Experiment: Unraveling Stress’s Impact on Neurons
In a study titled "Stress Dynamically Modulates Neuronal Autophagy to Gate Depression Onset," published in the esteemed journal Nature, researchers used both in vivo and in vitro experiments to explore how stress and antidepressants influence autophagy in the lateral habenula. They subjected mouse models to different stressors, including restraint and social defeat, to assess the effects.
Acute vs. Chronic Stress: A Tale of Two Responses
Results showed a dramatic contrast: acute stress heightened autophagy markers, leading to increased cleanup in the brain region, while chronic stress triggered the opposite. This research highlighted that proteins associated with autophagy were particularly downregulated in response to chronic stress, confirming a unique reaction in neurons of the lateral habenula.
Antidepressants: A New Hope for Neural Recovery
The team tested various antidepressants, including paroxetine and ketamine, finding that these medications could restore autophagy function, particularly in the stressed mice. However, when autophagy was blocked, the beneficial effects of antidepressants vanished, suggesting a crucial link between autophagy and mood stabilization.
Reversing Depression: The Power of Autophagy Enhancement
Mice lacking key autophagy genes displayed signs of depression, such as reduced social interaction. Remarkably, using a Beclin-1 activating peptide could reverse these behaviors swiftly, marking the potential for rapid treatment options. This peptide not only mitigated depression-like symptoms but also inhibited the onset during stress exposure.
The Future of Antidepressants: Targeting Autophagy
The findings indicate that promoting autophagy in the lateral habenula could be a game-changer in mental health treatment. By targeting this mechanism, researchers hope to develop faster-acting antidepressants that tackle the core issues of stress-induced depression. This revolutionary insight positions lateral habenula autophagy as a vital gatekeeper between stress and depression, paving the way for innovative therapeutic strategies.
In summary, this research not only sheds light on the complex relationship between stress and depression but also opens avenues for rapid interventions in mental health care.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)