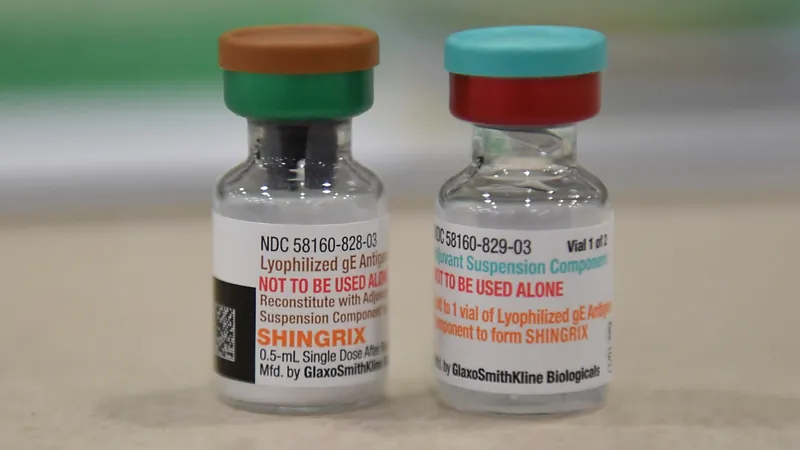
Shingles Vaccine: A Surprising Ally Against Dementia?
2025-05-05
Author: Ming
Exciting new research suggests that the shingles vaccine may not just prevent a painful rash but could also play a significant role in delaying or even preventing dementia.
A groundbreaking study published in the journal JAMA on April 23 analyzed electronic health records across Australia. Researchers discovered that older adults eligible for the free shingles vaccine were dramatically less likely to be diagnosed with dementia over a 7.4-year period compared to those just too old for the program.
The Viral Connection: Unraveling Alzheimer’s Mystery
These intriguing findings bolster the "viral hypothesis" of Alzheimer's disease, which suggests that viral infections, particularly those from the herpesvirus family—including the varicella-zoster virus responsible for chickenpox and shingles—could contribute to the development of dementia. If further research confirms these results, we may already have an effective and affordable tool to combat dementia on hand.
Dr. Sten Vermund, Dean of the University of South Florida College of Public Health, highlighted the strength of these findings, asserting that it’s challenging to pinpoint any factor other than the vaccine as the reason behind the observed protective effect.
How the Study Worked: A Unique Approach
Unlike typical studies, which require costly and complex clinical trials, this research leveraged a unique situation in Australia. The government initiated a shingles vaccination program on November 1, 2016, targeting adults aged 70 to 79, creating nearly an experiment-like scenario where eligible individuals became a new cohort to analyze.
Dr. Pascal Geldsetzer, Senior Author of the study, emphasized that the age cutoff created a natural division, allowing them to compare those eligible for vaccination against those slightly older who were not.
Impressive Findings: Shingles Vaccine's Impact
The analysis reviewed data from over 101,200 patients, revealing that individuals eligible for the shingles vaccine had a 1.8% lower rate of dementia diagnoses compared to their ineligible counterparts. Specifically, 3.7% of those vaccinated were diagnosed with dementia, versus 5.5% of those not vaccinated. This remarkable effect appeared unique to dementia, with no increase in other chronic health issues, reinforcing the vaccine's protective role.
Beyond Correlation: Seeking More Answers
Previous research from Geldsetzer's team in Wales had already indicated a 20% lower rate of dementia diagnoses among vaccinated individuals. While Dr. Logan DuBose pointed out the modest difference in the Australian study, the consistency across two well-researched studies is compelling.
Experts emphasize the need for more extensive research. Questions remain, such as whether the vaccine's effects might vary across different genetic backgrounds, particularly concerning the APOE4 gene linked to dementia.
Future studies are imperative to unravel the mechanisms behind the shingles vaccine's potential protective effects against dementia, with some hypotheses suggesting that preventing the reactivation of the varicella-zoster virus might impede brain damage.
A Call for Further Research
Now, Dr. Geldsetzer and his team are actively seeking funding to conduct a formal clinical trial to definitively test the shingles vaccine's impact on dementia prevention. With the stakes this high, the implications could be revolutionary for public health.
Stay tuned for updates on this remarkable and potentially life-changing line of research!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)