Revolutionizing Obesity Treatment: The Power of Targeting GLP-1 in the Brain
2025-06-02
Author: Li
A Breakthrough in Hunger Regulation
For years, scientists have grappled with how our bodies manage hunger and fullness, and a key player in this complex system is glucagon-like peptide 1 (GLP-1). Initially recognized for its blood sugar-regulating properties, GLP-1's influence on appetite is far more intricate than previously thought. Professor Stefan Trapp from University College London is at the forefront of this exciting research, revealing that GLP-1 is produced not just in the gut but also in the brain, and the mechanisms at play are surprisingly different.
Rethinking the Gut-Brain Connection
The traditional view of GLP-1 was straightforward: food enters the gut, triggers GLP-1 release, which then travels to the brain to suppress appetite. However, Trapp's groundbreaking findings reveal a vital oversight: PPG neurons, responsible for producing GLP-1 in the brainstem, do not respond to circulating GLP-1 from the gut. Instead, the brain's GLP-1 system functions autonomously, reacting to signals like stomach distention and neurological inputs.
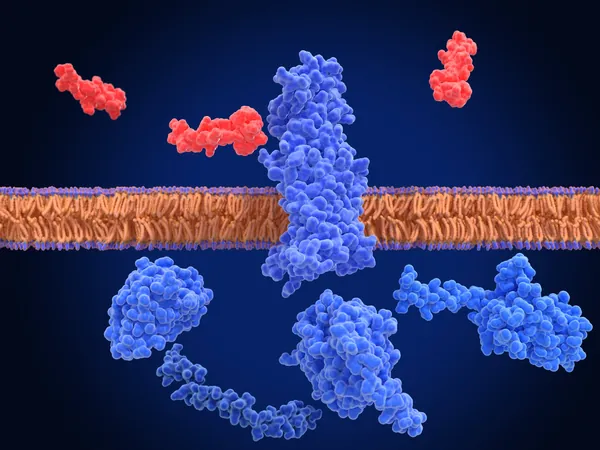
Two-Dimensional Action: Hormones vs. Neurotransmitters
GLP-1 operates in two distinct modes: as a hormone in the bloodstream, enhancing insulin response, and as a neurotransmitter in the brain, offering localized signaling. Trapp elucidates this dual action: peripheral GLP-1 floods the body, while central GLP-1 operates with pinpoint precision, affecting specific brain areas without triggering widespread changes.
Navigating the Blood-Brain Barrier: A Major Hurdle
The blood-brain barrier presents a significant challenge for GLP-1 treatment development. Trapp emphasizes its protective role against harmful substances while also complicating drug delivery. His studies suggest that both the peripheral and central GLP-1 systems may function independently, necessitating tailored therapeutic approaches.
Evidence Uncovers Distinct Roles of GLP-1
Research supports the theory of independent GLP-1 systems. Key findings include the rapid breakdown of peripheral GLP-1 and the successful appetite suppression observed when directly targeting central GLP-1 neurons. Moreover, combining peripheral and central GLP-1 treatments has shown enhanced effectiveness in reducing hunger.
Exploring New Therapeutic Horizons
The promise of central GLP-1 as a therapeutic target is monumental. Trapp's animal studies indicate that stimulating brain GLP-1 can significantly reduce food intake for several hours. However, creating drugs that effectively target these pathways for prolonged periods remains a challenge due to the blood-brain barrier.
Addressing Side Effects: The Nausea Dilemma
Another aspect of Trapp's research addresses the side effects of existing GLP-1 receptor agonists, notably nausea. Current treatments do not only impact appetite; they trigger reactions in sensitive areas of the brain. This highlights the need to refine drug development to enhance efficacy while minimizing adverse effects.
Charting the Future: Targeted Solutions to Obesity
As research progresses, understanding the nuanced roles of GLP-1 will be key to combating obesity. Future therapies may target specific GLP-1 receptor populations within the brain, tapping into mechanisms beyond appetite regulation and addressing subconscious food cues. Professor Trapp's pioneering work is steering us toward innovative obesity treatments that promise both safety and effectiveness.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)