Revolutionizing COPD Diagnosis: A New Era of Detection
2025-05-22
Author: Sarah
A Breakthrough in COPD Understanding
Researchers at the University of Alabama at Birmingham have unveiled a groundbreaking framework for diagnosing chronic obstructive pulmonary disease (COPD), paving the way for earlier detection of individuals at risk for severe respiratory issues who may otherwise slip through the cracks of standard diagnostic criteria.
The COPD Crisis
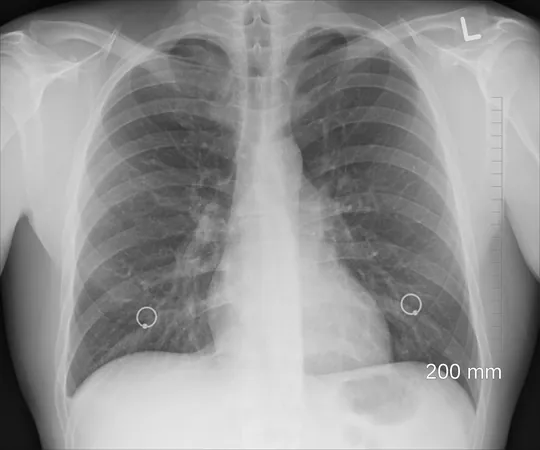
With a staggering 392 million people affected worldwide, COPD stands as a leading cause of disability and death. Traditionally, diagnosis relied heavily on spirometry, specifically using a forced expiratory volume to forced vital capacity ratio (FEV1/FVC) of less than 0.70 as the definitive metric. However, research shows this narrow focus often overlooks individuals with significant symptoms and structural lung damage.
The Hidden Sufferers
Imaging studies have revealed that even those who don’t show airflow obstruction could still be battling emphysema or bronchial wall thickening. This is especially true for smokers, who often experience troubling respiratory symptoms and diminished quality of life.
A Multidimensional Approach
In their study, published in JAMA, the researchers called for a holistic, multidimensional diagnostic method that combines respiratory symptoms with chest CT findings. This reshaped structure could uncover additional COPD cases and better predict health outcomes.
Research Findings Unveiled
The study pooled data from two extensive cohorts. The COPDGene study gathered 10,305 participants in the U.S., while CanCOLD enrolled 1,561 Canadians, both groups followed for years. Each participant underwent spirometry and CT imaging, leading researchers to a diagnostic framework categorized by airflow obstruction and a series of minor criteria.
New Diagnoses and Implications
From the COPDGene group, 811 individuals without airflow obstruction were newly diagnosed with COPD based solely on minor criteria, showing significantly worse health outcomes. In the CanCOLD cohort, a small percentage without airflow obstruction were similarly reclassified, indicating the need for this evolved diagnostic path.
Transforming Healthcare for COPD Patients
The study's authors emphasize that recognizing structural lung abnormalities and respiratory symptoms can signal worse health outcomes, even when spirometry results are normal. This new diagnostic model doesn’t dismiss spirometry but enriches it with additional criteria, enhancing clinicians' ability to identify COPD.
A Call for Change in Public Health
This revolutionary approach could transform how healthcare professionals detect and manage early or atypical cases of COPD. It holds particular promise for improving diagnostic equity, especially for Black individuals often diagnosed with emphysema without airflow obstruction.
As the awareness of this compelling multidimensional framework spreads, we may see a significant leap in timely diagnoses—ultimately saving lives.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)