Revolutionary Study Unveils Hidden Truths About Diabetes and Heart Procedures
2025-04-21
Author: Ming
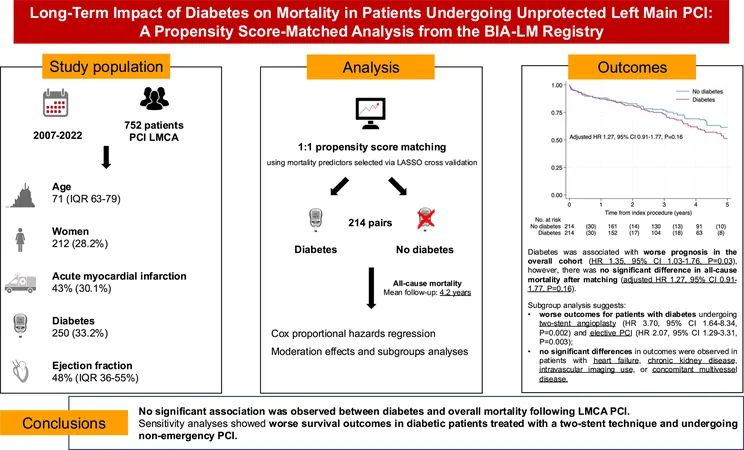
A groundbreaking analysis from the BIA-LM registry is shaking up our understanding of diabetes in patients undergoing left main coronary artery (LMCA) procedures. The findings reveal that while diabetes patients initially showed lower five-year survival rates, after adjusting for other health conditions, the differences in mortality rates disappeared. This suggests that it's not diabetes itself that heightens the risk but rather associated comorbidities.
These insights agree with previous research from major trials—NOBLE, EXCEL, SYNTAX, and PRECOMBAT—pointing to elevated all-cause mortality among diabetes patients requiring revascularization for LMCA disease. Strikingly, those with diabetes showed increased cardiovascular death rates, especially if they had complex anatomical structures.
Understanding Insulin Dependency: Impact on Outcomes
Diving deeper, the study found no significant differences in long-term outcomes between insulin-dependent and non-insulin-dependent diabetes patients, challenging some prior assumptions. Recent meta-analyses echo this, revealing that insulin therapy does not significantly elevate risks for adverse cardiovascular events or general mortality.
Trial Design Matters: A Closer Look
However, interpreting these results is complex due to trial biases and evolving treatment methods. Past studies included patients deemed equally suitable for various treatment methods, limiting how these findings translate to everyday practice. Techniques have advanced dramatically since those trials, with new-generation drug-eluting stents and improved procedural techniques leading to significantly better outcomes. Contrast this with much lower rates of intravascular imaging observed in contemporary data, signifying a shift in procedural standards.
Diabetes and the Two-Stent Technique: A Mixed Bag
Another fascinating finding pertains to the two-stent technique in bifurcation cases. Non-diabetic patients navigating this route showcased superior survival rates compared to their diabetic counterparts. Existing research highlights the troubled outlook for diabetics in these complex scenarios, urging for more focused studies.
The Gender Gap: A Broader Perspective
While examining gender dynamics, the study noted that women represented only 28.2% of patients undergoing LMCA interventions, a trend aligning with broader population data. Historically, women have faced significant rates of major cardiac events, but mortality rates post-PCI appeared equitable across sexes in this cohort.
Myocardial Infarctions: A Paradoxical Survival Advantage
Interestingly, diabetic patients who experienced myocardial infarctions (MI) often survived longer than their non-diabetic peers. This counterintuitive outcome could be tied to the younger age at MI onset for diabetics, which suggests they might possess more physiological resilience and better collateral circulation.
Heart Failure and Chronic Kidney Disease: The Complications Deepen
When factoring in other comorbid conditions, the study didn’t find substantial survival differences between diabetic and non-diabetic patients facing multiple coronary issues. However, earlier research frequently indicates more severe coronary disease in diabetic populations, raising questions about treatment strategies.
The Call for More Research: A Growing Need
With an aging population and shifting health dynamics, there's a pressing need for expansive clinical trials focusing on the long-term outcomes of PCI in diabetes. The findings highlight a significant cohort of high-risk patients that could benefit from tailored revascularization strategies.
Final Thoughts: Strengths and Limitations of the Study
While this study provides profound insights, it also has limitations typical of observational research, necessitating cautious interpretation. Though propensity score matching helped minimize confounding factors, unmeasured variables might still skew results. Furthermore, with advancements in treatment and critiques on the use of the SYNTAX score in clinical decisions, it remains crucial to approach these findings with a comprehensive understanding of their context.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)