Revolutionary Study Reveals Breakthrough in Treating Platinum-Resistant Ovarian Cancer
2025-04-04
Author: Arjun
Groundbreaking Study Overview
A groundbreaking study conducted by researchers at the University of Cincinnati Cancer Center has unveiled a revolutionary approach to treating platinum-resistant ovarian cancer, a condition where patients experience recurrence shortly after receiving platinum-based chemotherapy. The findings, led by Dr. Thomas Herzog, highlight how personalized treatment strategies based on a novel testing platform could significantly improve patient outcomes.
Understanding Platinum-Resistant Ovarian Cancer
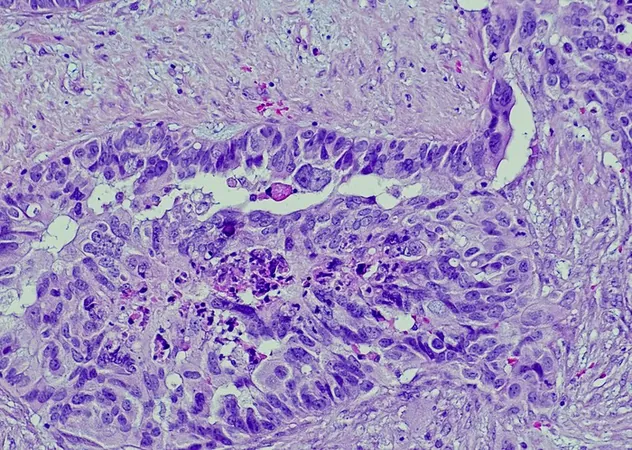
Dr. Herzog, a renowned physician and researcher at the Cancer Center, explained that epithelial ovarian cancer often initially responds well to chemotherapy. However, this response can be undermined as cancer stem cells (CSCs) begin to repopulate and repair the tumor post-treatment. "This resistance to therapy arises partly from the selection and reactivation of CSCs, which rebuild the tumor despite the damage inflicted by chemotherapy," he said, emphasizing the critical role these cells play in cancer recurrence.
The ChemoID Platform
The ChemoID platform, co-developed by Dr. Pier Paolo Claudio, represents a significant advancement in identifying the most effective anticancer drugs for individual patients. By testing tumor samples against specific drugs, the platform can predict which treatments will be most beneficial, specifically targeting both tumor cells and the resilient cancer stem cells.
Trial Results
In the trial, 81 patients diagnosed with platinum-resistant ovarian cancer were randomized to receive treatment via either the innovative ChemoID platform or standard physician-chosen methods. Traditional approaches generally rely on a mix of approved therapies and physicians’ past experiences without the tailored insight ChemoID offers.
The researchers measured the success of these treatments based on the objective response rate (ORR)—the percentage of participants who showed a partial or complete response—as well as progression-free survival (PFS) and the duration of treatment response. The results were striking: the ChemoID group achieved an ORR of 50%, a stark contrast to just 5% in the standard treatment group. Furthermore, patients treated through ChemoID experienced a median PFS of 11 months, while those receiving conventional treatment had a median of only three months.
Implications for Healthcare
The implications of these results extend beyond patient survival; they signify potential cost savings in healthcare. Dr. Claudio noted that improved treatment response rates could lead to reduced healthcare costs by minimizing the use of ineffective therapies and unnecessary toxicities, relieving patients of the financial burden associated with extensive treatments.
Future Research
Looking ahead, Dr. Herzog emphasized the need for further research to validate the ChemoID platform and to explore its application in various molecular subgroups, including patients with BRCA mutations. The ongoing investigation into emerging biologic therapies will further refine the application of this promising test, potentially transforming the landscape of treatment for ovarian cancer.
Conclusion
As researchers continue to unlock the complexities of cancer treatment, this study stands as a beacon of hope, suggesting that personalized medicine could soon become the gold standard for combating even the most resistant forms of ovarian cancer.
Stay tuned as we follow this pivotal research journey and its implications for the future of cancer care!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)